Case Report: Hypoalbuminemia in a 61-Year-Old Patient – Albumin Level 2.1 g/dL on Presentation
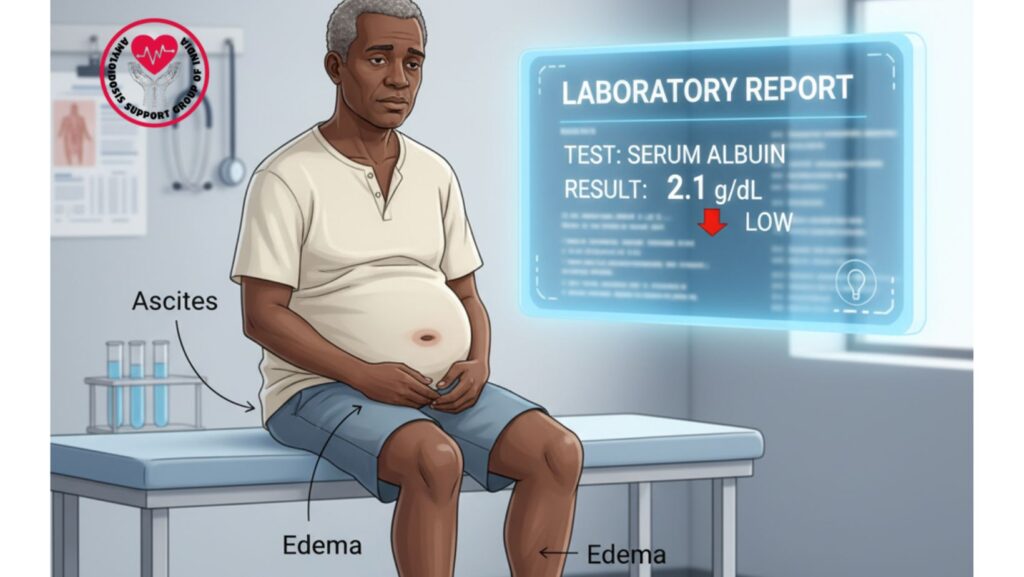
Table of Contents
Introduction
Serum albumin is perhaps the most important laboratory indicator in clinical medicine. Produced by the liver, albumin is responsible for sustaining oncotic pressure, carrying hormones, fatty acids, and drugs, and is an indicator of a patient’s overall nutritional and systemic health.
If serum albumin decreases below the normal value (3.5–5.5 g/dL), the state is called hypoalbuminemia. It can result from liver disease, kidney disease, malnutrition, or systemic protein loss, and it can frequently act as an important prognostic factor in chronic conditions.
This case presentation brings to fore a 61-year-old African-American male who came in with an albumin level of 2.1 g/dL, along with other systemic findings indicative of amyloidosis. We shall discuss his clinical presentation, diagnostic results, differential diagnosis, and management strategy, as well as the general significance of hypoalbuminemia.
Patient Profile
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Comorbidities: Hypertension, mild diabetes
- Presenting Symptoms: Progressive leg swelling, abdominal distension, fatigue, weight loss
Initial Presentation
The patient complained of:
- Swelling of the legs (bilateral, progressive, pitting edema)
- Abdominal distension due to tense ascites
- Fatigue and weakness
- Early satiety and loss of appetite
- Shortness of breath on exertion (mild)
Physical exam was notable for: - Bilateral lower extremity edema
- Tense ascites with fluid thrill
- Jugular venous distention (JVD)
- Mild hepatomegaly
Laboratory Findings
- Serum Albumin: 2.1 g/dL (markedly low)
- CBC: Mild normocytic anemia
- Kidney Function: Increased creatinine, decreased eGFR
- Liver Function Tests: Mild elevation of enzymes, hypoalbuminemia
- Urinalysis: Presence of proteinuria
- Serum Protein Electrophoresis (SPEP): M-spike
- Immunofixation: Presence of light chains (indicative of AL amyloidosis)
Pathophysiology of Hypoalbuminemia
Albumin is produced by the liver and accounts for almost 50–60% of plasma protein. The patient’s low level of 2.1 g/dL reflects an important disturbance.
Mechanisms of Hypoalbuminemia:
- Decreased Synthesis: In cases of chronic liver disease or malnutrition.
- Increased Loss: Nephrotic syndrome (kidney disease) or protein-losing enteropathy.
- Increased Catabolism: Inflammatory conditions increase breakdown of albumin.
- Dilutional Effect: Overload of fluids artificially lowers measured albumin.
In this patient, the most probable contributors were:
- Renal protein loss (amyloidosis with proteinuria)
- Hepatic involvement due to amyloid infiltration
- Systemic inflammation
Differential Diagnosis Considered
Prior to establishing amyloidosis, clinicians also considered other causes:
- Cirrhosis of the Liver – frequently accompanied by ascites and low albumin.
- Nephrotic Syndrome – an old cause of hypoalbuminemia and edema.
- Congestive Heart Failure – may result in ascites, JVD, and edema.
- Protein-Losing Enteropathy – loss of proteins through the intestine.
The presence of monoclonal protein, renal involvement, and cardiac manifestations indicated amyloidosis.
Diagnostic Confirmation
- Echocardiogram: Diastolic dysfunction, thickening of ventricles
- Cardiac MRI: Restrictive cardiomyopathy as a result of amyloid infiltration
- Abdominal Ultrasound: Ascites, hepatomegaly
- Fat Pad Biopsy: Congo red positive for amyloid (apple-green birefringence under polarized light)
- Bone Marrow Biopsy: Plasma cell dyscrasia consistent with AL amyloidosis
Final Diagnosis
Systemic AL Amyloidosis with renal and cardiac involvement, presenting with hypoalbuminemia (albumin 2.1 g/dL), edema, ascites, and JVD.
Clinical Significance of Low Albumin (2.1 g/dL)
- Severe Hypoalbuminemia: Normal range is 3.5–5.5 g/dL. A level of 2.1 g/dL indicates advanced systemic disease.
- Prognostic Indicator: Low albumin is highly associated with adverse outcome in cardiac and renal amyloidosis.
- Edema and Ascites: Directly linked to decreased oncotic pressure.
- Drug Binding & Metabolism: Several drugs are bound by albumin; low levels change pharmacokinetics.
- Marker of Disease Burden: Indicates multi-organ dysfunction.
Management
1. Supportive Measures
- Restriction of salt to decrease fluid overload
- Diuretics (furosemide, spironolactone) in edema and ascites
- Albumin infusions in severe symptomatic hypoalbuminemia
- Nutritional supplementation with high-protein diet
2. Disease-Specific Treatment
- Chemotherapy (CyBorD regimen: Bortezomib, Cyclophosphamide, Dexamethasone)
- Autologous Stem Cell Transplantation – reserved for eligible patients
- Novel drugs (Daratumumab, CAEL-101) under consideration
3. Monitoring
- Albumin levels every 4–6 weeks
- Renal function studies for progression
- Cardiac monitoring with BNP and echocardiography
Patient Outcome
- Following initiation of treatment, edema decreased, and albumin modestly improved to 2.6 g/dL.
- Ascites needed recurrent paracentesis initially, subsequently managed with diuretics.
- Cardiac symptoms stabilized with supportive care.
- Patient had increased appetite, mobility, and energy.
Clinical Insights
For Clinicians
- Always pursue hypoalbuminemia < 2.5 g/dL since it typically indicates severe systemic disease.
- Combining physical findings + laboratory markers is critical in the diagnosis of uncommon diseases.
- In amyloidosis, low albumin tends to indicate both renal as well as hepatic involvement.
For Patients and Families
- Low albumin is not merely a blood test result, but an indicator of severity of disease.
- Symptoms such as swelling, weakness, and bloating must not be disregarded.
- Quality of life may be enhanced by treatment even if the disease cannot be treated.
- Patient support groups (such as Amyloidosis Support India) are important in education and support.
Broader Implications
Hypoalbuminemia is usually undervalued as merely a “routine laboratory result.” Yet, as in this case, it may be the first key indication of systemic disease. In amyloidosis, it indicates multi-organ involvement and protein loss, and thus serves as a significant diagnostic and predictive marker.
Increased vigilance on the part of both healthcare workers and patients can result in earlier detection, timely treatment, and improved outcomes.
Conclusion
This case presentation of a 61-year-old African-American man with an albumin concentration of 2.1 g/dL stresses the significance of identifying hypoalbuminemia as a red flag. It is not only a laboratory finding but also a window into systemic burden of disease.
With the integration of attentive clinical assessment, focused testing, and prompt therapy, patients with amyloidosis and other etiologies of hypoalbuminemia can attain enhanced survival and quality of life.

