Case Report: Normal INR and Creatinine in a 61-Year-Old Patient – Clinical Insights on Presentation
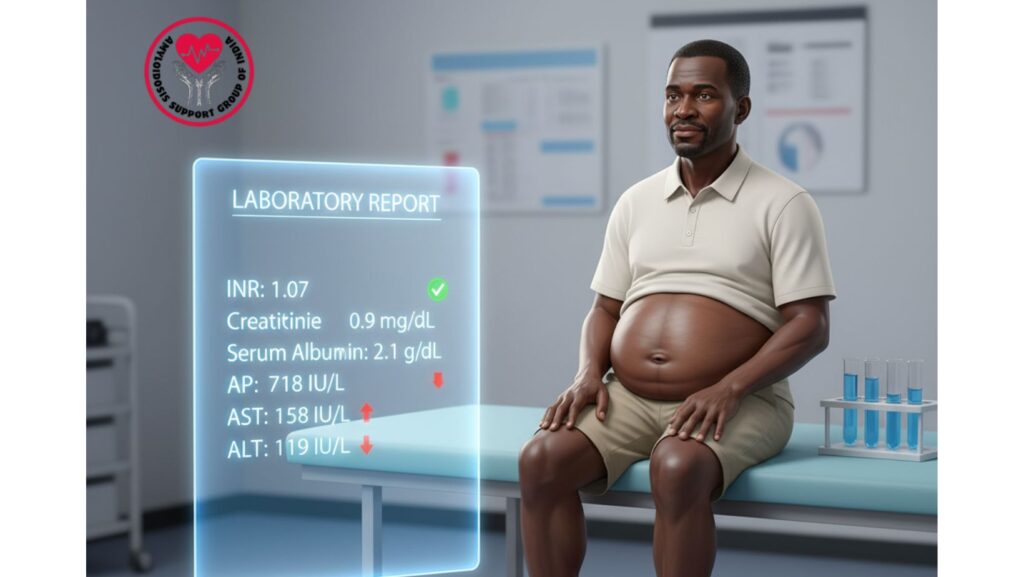
Table of Contents
Introduction
International Normalized Ratio (INR) and serum creatinine are key laboratory parameters of clinical medicine.
- INR evaluates blood coagulation, the extrinsic pathway specifically, and is a sensitive marker for liver synthetic function and monitoring for anticoagulation therapy.
- Serum creatinine indicates renal function and glomerular filtration rate (GFR) and is key to information regarding the health of the kidneys.
In systemic illness like amyloidosis, liver and renal involvement is frequent, and laboratory abnormalities may precede organ dysfunction. The patient in this case, however, presented with normal INR (1.07) and creatinine (0.9 mg/dL) despite other evidence of systemic disease.
The case underscores the need for comprehensive evaluation, wherein normal renal and coagulation markers do not rule out systemic disease but are useful in assessing organ function and prognosis.
Patient Profile
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Relevant Medical History: Hypertension, mild diabetes
- Presenting Symptoms: Leg swelling, abdominal distension, fatigue, shortness of breath
Clinical Presentation
The patient complained of:
- Bilateral lower limb edema over a few months
- Abdominal distension (ascites)
- Fatigue and weakness
- Early satiety and mild weight loss
- Shortness of breath on exertion
Physical Examination Findings: - Pitting edema of lower extremities
- Tense ascites with fluid thrill
- Jugular venous distension (JVD)
- Slight hepatomegaly
- No jaundice or acute bleeding signs
Laboratory Findings
- INR: 1.07 (normal: 0.8–1.2)
- Serum Creatinine: 0.9 mg/dL (normal: 0.6–1.3 mg/dL)
- Albumin: 2.1 g/dL (hypoalbuminemia)
- Total Bilirubin: 0.5 mg/dL
- Alkaline Phosphatase (AP): 718 IU/L
- AST: 158 IU/L
- ALT: 119 IU/L
- Serum Protein Electrophoresis (SPEP): Monoclonal light chain detected
- Urinalysis: Mild proteinuria
Significance of Normal INR
- INR expresses extrinsic coagulation pathway efficacy and is affected by vitamin K-dependent coagulation factors, which are primarily produced by the liver.
- Normal INR (1.07) expresses:
- Maintenance of liver synthetic function even in the presence of mild elevations of enzymes.
- Lack of severe coagulopathy.
- Safety for the performance of procedures requiring normal coagulation.
In amyloidosis, normal INR indicates that hepatic infiltration has not significantly impaired synthetic function.
Significance of Normal Creatinine
- Serum creatinine is a marker of glomerular filtration rate and kidney health.
- Normal creatinine (0.9 mg/dL) signifies:
- Normal kidney function at presentation.
- Absence of important nephrotic-range proteinuria impacting renal clearance.
- Baseline kidney status for treatment purposes.
In spite of proteinuria and hypoalbuminemia, the filtering ability of the kidney was maintained, indicative of early or mild renal involvement.
Interpretation in Context
Though the patient had:
- Edema
- Ascites
- Hypoalbuminemia
- Increased liver enzymes
The normal INR and creatinine signaled:
- Early-stage organ involvement – liver and kidneys were functionally normal.
- Favorable prognosis markers – intact synthetic and filtration function ensures safe use of chemotherapeutic drugs.
- Guidance for therapy – intensive therapies like Bortezomib, Cyclophosphamide, Dexamethasone, or stem cell transplant are safer with normal INR and creatinine.
Differential Diagnosis
- Systemic Amyloidosis – most akin to multi-organ presentation.
- Chronic Liver Disease – early involvement may maintain INR in spite of enzyme rise.
- Renal Disease / Nephrotic Syndrome – hypoalbuminemia is present without creatinine rise in the initial stages.
- Cardiac Involvement – edema and ascites can also be caused by heart failure.
Diagnostic Workup
- Ultrasound Abdomen: Moderate ascites, hepatomegaly, normal kidneys.
- Echocardiography: Restrictive cardiomyopathy consistent with cardiac amyloidosis.
- Fat Pad Biopsy: Congo red positive for amyloid.
- Bone Marrow Biopsy: Plasma cell dyscrasia confirming AL amyloidosis.
- Serial Labs: Tracked INR, creatinine, LFTs, and albumin trends.
Management
Supportive Care
- Diuretics to manage edema and ascites
- Salt restriction
- Nutritional support for hypoalbuminemia
Disease-Specific Therapy
- CyBorD regimen (Bortezomib + Cyclophosphamide + Dexamethasone)
- Stem Cell Transplant in eligible patients
- Novel therapies such as Daratumumab for refractory patients
Monitoring
- Serial INR and coagulation panels
- Serial creatinine and eGFR monitoring
- Levels of liver enzymes and albumin
- Cardiac function evaluation
Patient Outcome
- At 6 months:
- INR was normal, enabling continuation of chemotherapy safely.
- Creatinine was stable, reflecting maintained renal function.
- Edema and ascites were improved with supportive care.
- Albumin increased modestly, liver enzymes decreased.
- Quality of life was improved overall.
Clinical Insights
For Clinicians
- Normal INR and creatinine do not exclude systemic disease, but demonstrate maintained organ function.
- Early diagnosis of amyloidosis makes possible timely therapy before destructive changes occur.
- Follow trends over time; an abrupt increase in INR or creatinine can indicate progressive hepatic or renal disease.
For Patients and Families
- Normal laboratory values may be reassuring, but frequent follow-up is necessary.
- Multi-organ diseases such as amyloidosis necessitate holistic care and management.
- Early intervention enhances outcomes even if initial laboratory values are normal.
Broader Implications
This case emphasizes the value of contextual interpretation of lab work:
- Normal INR and creatinine in systemic amyloidosis can indicate early organ involvement.
- These findings are useful for risk stratification and treatment planning.
- The convergence of clinical findings, labs, imaging, and biopsy ensures correct diagnosis and monitoring.
Conclusion
The 61-year-old African-American man with normal INR (1.07) and creatinine (0.9 mg/dL) illustrates that retained liver and kidney function may be associated with systemic amyloidosis.
These markers are useful in:
- Providing insight into severity of disease
- Facilitating choice of treatment
- Providing prognostic information for long-term care
Monitoring regularly and early intervention are important to preserve organ function and enhance quality of life in systemic amyloidosis patients.

