Case Report: Nephrotic-Range Proteinuria in a 61-Year-Old Patient – Clinical Implications
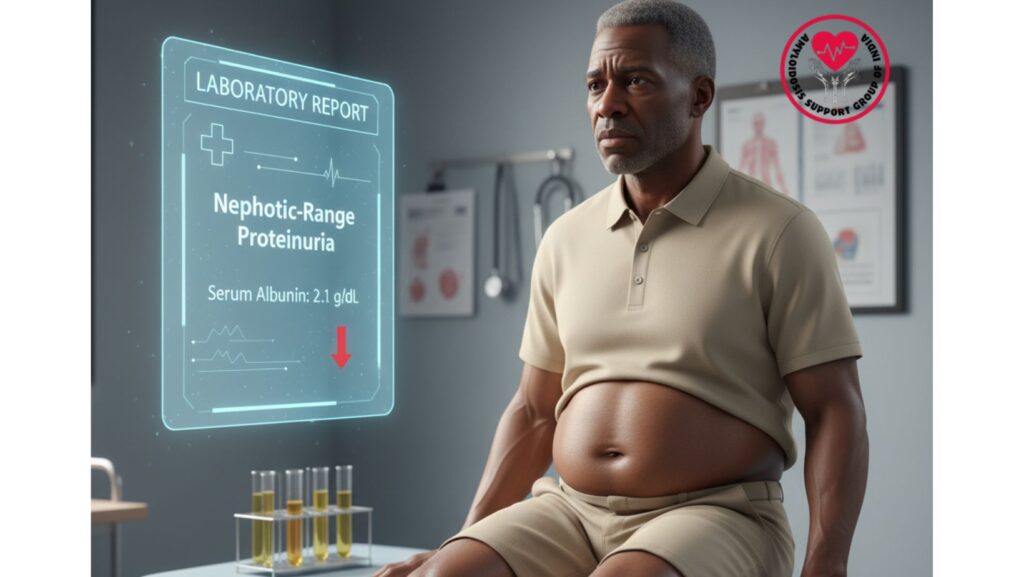
Table of Contents
Introduction
Proteinuria is a characteristic of renal impairment, reflecting abnormal urinary loss of protein. When urinary loss is more than 3.5 g/day, it is termed nephrotic-range proteinuria and is frequently seen with hypoalbuminemia, edema, hyperlipidemia, and enhanced risk of thromboembolism.
In systemic illnesses such as amyloidosis, nephrotic-range proteinuria is an usual presentation of renal involvement, which is indicative of amyloid fibril infiltration of the glomeruli. Early detection is important, as it informs diagnosis and management of the primary disease.
This case reports a 61-year-old African-American man with nephrotic-range proteinuria, in addition to other systemic manifestations, and reviews the clinical, diagnostic, and management issues.
Patient Profile
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Relevant Medical History: Mild diabetes, hypertension
- Presenting Symptoms: Abdominal distension, bilateral leg swelling, fatigue
Clinical Presentation
The patient complained of:
- Progressive bilateral leg swelling (edema) over 2–3 months
- Abdominal distension (ascites) with pain
- Fatigue and weakness in general
- Shortness of breath (mild)
Physical Examination Findings:
- Bilateral pitting edema of lower extremities
- Ascites with positive fluid wave
- Jugular venous distension
- Mild hepatomegaly
- No jaundice or acute distress
Laboratory Findings
- Urinalysis: Severe proteinuria (>3.5 g/day), ascertaining nephrotic range
- Serum Albumin: 2.1 g/dL (hypoalbuminemia)
- Total Bilirubin: 0.5 mg/dL
- Alkaline Phosphatase (AP): 718 IU/L
- AST: 158 IU/L
- ALT: 119 IU/L
- INR: 1.07 (normal)
- Creatinine: 0.9 mg/dL (normal)
- Serum Protein Electrophoresis: Monoclonal light chain identified
- Immunofixation: Establishes AL amyloidosis
Pathophysiology of Nephrotic-Range Proteinuria
Nephrotic-range proteinuria results when the glomerular filtration barrier is highly compromised, permitting considerable plasma protein leakage into the urine.
In systemic AL amyloidosis:
- Amyloid fibrils accumulate in glomeruli, mesangium, and basement membranes.
- Resulting in increased glomerular permeability and extensive loss of protein.
- Hypoalbuminemia ensues from urinary loss of albumin greater than hepatic production.
- Edema and ascites due to decreased plasma oncotic pressure.
- Secondary hyperlipidemia can occur as a compensatory hepatic response.
Clinical Significance
- Nephrotic-range proteinuria is an early sign of renal involvement in systemic amyloidosis.
- Indicates progressive renal disease if left untreated.
- Complications associated with it:
- Edema and ascites
- Hypoalbuminemia
- Hypercoagulability (thromboembolic risk)
- Increased cardiovascular risk
Differential Diagnosis
- Primary Glomerular Disease – Minimal change disease, focal segmental glomerulosclerosis, membranous nephropathy.
- Secondary Glomerular Disease – Diabetes mellitus, lupus nephritis, amyloidosis.
- Chronic Kidney Disease (CKD) – Can produce proteinuria, typically less than nephrotic range in the early stages.
- Systemic Amyloidosis – Most in keeping with multi-organ disease and monoclonal light chains.
Diagnostic Workup
- Urine Protein Quantification: 24-hour urine collection established nephrotic-range proteinuria.
- Renal Ultrasound: Kidneys of normal size and echotexture; no obstruction.
- Renal Biopsy:
- Congo red positive for amyloid deposition
- Electron microscopy established fibrillar deposits
- Serum Protein Electrophoresis (SPEP): Detected monoclonal light chain
- Cardiac Evaluation: Echocardiogram revealed restrictive cardiomyopathy
- Liver Evaluation: Mildly increased enzymes, normal bilirubin and INR
Management
Supportive Therapy
- Diuretics for edema and ascites control
- Salt restriction
- ACE inhibitors/ARBs to control proteinuria and preserve kidneys
- Nutritional support with protein intake within normal range
Disease-Specific Therapy
- Chemotherapy: CyBorD regimen (Bortezomib, Cyclophosphamide, Dexamethasone)
- Stem Cell Transplantation in suitable patients
- New Therapies: Daratumumab, CAEL-101 in relapsed cases
Monitoring
- Serial urine protein measurements
- Renal function tests: Creatinine, eGFR
- Albumin levels for nutritional status as well as hydration
- Blood pressure and cardiovascular monitoring
Patient Outcome
- At 6 months of treatment:
- Proteinuria reduced but still in nephrotic range at first
- Edema and ascites resolved with diuretics
- Albumin modestly improved
- Renal function intact (creatinine was 0.9 mg/dL)
- Cardiac symptoms improved
- Overall quality of life enhanced
Clinical Insights
For Clinicians
- Systemic amyloidosis with nephrotic-range proteinuria indicates renal disease and disease severity.
- Early diagnosis permits prompt therapy before irreversible kidney damage.
- Renal biopsy, SPEP, and clinical correlation together is most important in diagnosis.
For Patients & Families
- Severe proteinuria can produce swelling and fluid retention even in the presence of normal kidney function.
- Urine protein, albumin, and renal function should be followed regularly.
- Lifestyle changes and support groups aid in symptom management and outcomes.
Broader Implications
This case highlights:
- The role of urinalysis in systemic disease diagnosis
- Early detection of renal involvement in amyloidosis can be used to influence treatment and outcome
- Multi-organ evaluation is necessary to prevent missed diagnosis
Conclusion
The 61-year-old African-American man with nephrotic-range proteinuria emphasizes the kidney presentation of systemic amyloidosis.
- Proteinuria, hypoalbuminemia, and edema portend glomerular involvement.
- Normal creatinine suggests early-stage renal disease, providing an opportunity for successful intervention.
- Thorough assessment, early treatment, and supportive therapy enhance outcomes and preserves quality of life.

