Case Report: Ascitic Fluid Analysis in a 61-Year-Old Patient – No Malignancy or Infection Identified
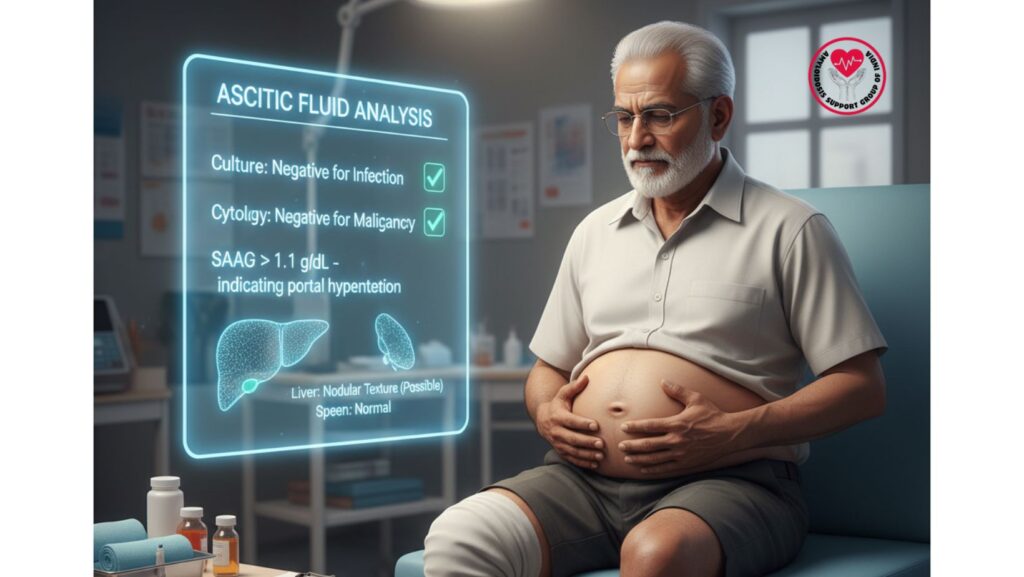
Table of Contents
Introduction
Ascitic fluid analysis is a critical diagnostic instrument for assessing fluid in the belly. When individuals have ascites, physicians need to identify if the fluid is secondary to:
- Infection (secondary peritonitis or spontaneous bacterial peritonitis)
- Malignancy (peritoneal metastatic disease or carcinomatosis)
- Portal hypertension (infiltrative liver disease, heart failure, cirrhosis)
Sterile, non-malignant ascitic fluid is more likely to represent systemic disease or portal hypertension than infection or cancer.
A 61-year-old African-American male with ascites who underwent paracentesis and had ascitic fluid negative for infection and cytology negative for malignancy directed the evaluation to systemic causes like amyloidosis.
Patient Profile
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Relevant Medical History: Hypertension, mild diabetes
- Presenting Symptoms: Progressive bilateral leg swelling, abdominal distension, fatigue
Clinical Presentation
The patient complained:
- Leg swelling (edema)
- Abdominal distension (ascites)
- Fatigue and early satiety
- Mild shortness of breath
Physical Examination Findings: - Pitting edema of the lower extremities
- Moderate ascites, positive fluid wave
- Jugular venous distention
- Mild hepatomegaly
- No jaundice or acute distress
Laboratory Findings
- Serum Albumin: 2.1 g/dL
- Ascitic Fluid Albumin: 0.8 g/dL
- SAAG: >1.1 g/dL (pointing towards portal hypertension)
- Liver Enzymes: Increased AP, AST, ALT
- INR: 1.07
- Creatinine: 0.9 mg/dL
- Nephrotic-range proteinuria
- Viral and autoimmune tests: Normal
- Serum Protein Electrophoresis (SPEP): Normal
Ascitic Fluid Analysis
Procedure
- Under sterile conditions, diagnostic paracentesis
- Fluid sent for:
- Cell count and differential
- Culture and Gram stain
- Cytology for malignancy
- Albumin measurement
Results
- Total cell count: Normal, no leukocytosis
- Culture: Negative for mycobacteria, fungi, or bacteria
- Cytology: No malignancy identified
- Albumin: 0.8 g/dL
- SAAG: 2.1 − 0.8 = 1.3 g/dL (>1.1 g/dL)
Interpretation
- Negative culture: No infection evidence, excluding spontaneous bacterial peritonitis (SBP)
- Negative cytology: No malignancy evidence in the peritoneum
- SAAG >1.1: Establishes portal hypertension as the etiology of ascites
Clinical Significance
- Excludes Infection
- Ascitic patients are at risk for spontaneous bacterial peritonitis (SBP), which may be fatal.
- Negative cultures enable clinicians to forego unnecessary antibiotics.
- Excludes Malignancy
- Peritoneal carcinomatosis or metastatic disease usually necessitates aggressive oncologic management.
- Negative cytology implies ascites is not cancer-related.
- **Confirms Portal Hypertension
- SAAG >1.1 signifies secondary ascites due to raised hydrostatic pressure in the portal venous system.
- Portal hypertension here was most likely due to early hepatic amyloidosis and/or cardiac involvement and not cirrhosis.
Diagnostic Correlation
- Clinical Signs: Edema, ascites, nephrotic-range proteinuria
- Imaging: Abdominal CT with ascites, possibly nodular liver, no hepatosplenomegaly
- Labs: Hypoalbuminemia, normal INR and bilirubin, elevated liver enzymes
- Ascitic Fluid: Sterile, non-malignant, SAAG >1.1
Conclusion: - Ascites is transudative, secondary to portal hypertension
- Infection and malignancy have been ruled out
- Attention turns to systemic amyloidosis evaluation
Causes of Non-Infectious, Non-Malignant Ascites
- Portal Hypertension
- Cirrhosis, restrictive cardiomyopathy, infiltrative liver disease (amyloidosis)
- Nephrotic Syndrome
- Severe hypoalbuminemia can cause accumulation of fluid
- Cardiac Ascites
- Right-sided heart failure or restrictive cardiomyopathy
Here, the association of portal hypertension (SAAG >1.1) and nephrotic-range proteinuria was suggestive of multi-organ systemic amyloidosis.
Management
Supportive Care
- Diuretics: Spironolactone and furosemide for ascites and edema
- Salt restriction: Fluid overload prophylaxis
- Nutritional support: Serum albumin maintenance
Disease-Specific Therapy
- Chemotherapy: CyBorD regimen (Bortezomib, Cyclophosphamide, Dexamethasone)
- Stem Cell Transplantation in selected patients
- Novel therapies: Daratumumab in refractory amyloidosis
Monitoring
- Serial paracentesis in recurrent ascites
- Liver function tests
- Monitoring of renal function and proteinuria
- Cardiac evaluation for restrictive cardiomyopathy
Outcome of Patient
The ascitic fluid was sterile and non-malignant
The SAAG >1.1 reaffirmed portal hypertension as active mechanism
Edema and ascites resolved with diuretics and systemic treatment
Liver and renal functions were stable
Overall quality of life was improved
Clinical Insights
For Clinicians
The analysis of ascitic fluid is crucial to exclude infection and malignancy
- SAAG calculation distinguishes ascites associated with portal hypertension from other etiologies
- Unremarkable results simplify management and prevent unnecessary therapy
For Patients & Families
- Sterile, non-neoplastic ascites usually results from systemic illness or heart/liver disease and not infection or cancer
- Follow-up and supportive care enhance symptom control and outcome
- Ascitic fluid result understanding reduces anxiety regarding infection or malignancy
Broader Implications
- Ascitic fluid analysis is a cornerstone in multi-organ disease evaluation
- Combining clinical findings, imaging, labs, and fluid analysis enhances diagnostic accuracy
- Early identification of systemic etiologies like amyloidosis enables early intervention and avoids complications
Conclusion
In this instance, the 61-year-old patient’s ascitic fluid was negative for infection and malignancy, and SAAG >1.1 established portal hypertension as the etiology of ascites.
- Malignancy and infection were ruled out, enabling attention to systemic amyloidosis
- Early detection and effective therapy enhanced fluid balance, organ function, and patient quality of life
Key Takeaway:
Ascitic fluid examination is important in diagnosing the etiology of ascites, directing management, and providing proper treatment for systemic illnesses such as amyloidosis.

