Case Report: Severe Liver Dysfunction on Readmission – Total Bilirubin 21.6 mg/dL, Elevated AP, AST, and ALT in a 61-Year-Old Patient
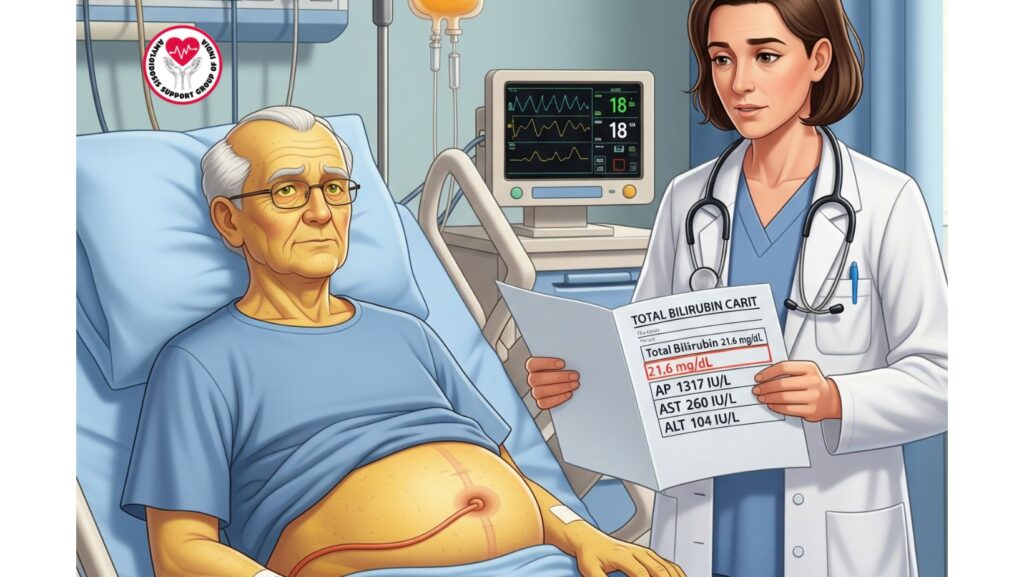
Table of Contents
Introduction
Systemic amyloidosis is an uncommon but causative illness involving many organs, including the liver. Hepatic amyloidosis tends to be insidious until end-stage dysfunction becomes apparent. This case presents the acute decline in liver function in a 61-year-old African-American man with primary (AL) amyloidosis, who was readmitted with jaundice, increasing ascites, and severely deranged liver function tests.
The report stresses the value of disease progression monitoring, early warning signs, and clinical significance of extensive liver involvement in systemic amyloidosis.
Patient Background
The patient first presented with:
- Subacute abdominal and leg swelling (for more than 2 months)
- Lower extremity edema bilaterally
- Tense ascites
- Jugular venous distension
Initial laboratory results were: - Albumin: 2.1 g/dL (low)
- AP: 718 IU/L (elevated)
- AST: 158 IU/L (elevated)
- ALT: 119 IU/L (elevated)
- Total Bilirubin: 0.5 mg/dL (normal initially)
- INR: 1.07
- Creatinine: 0.9 mg/dL
- Urinalysis: Nephrotic range proteinuria
Subsequent investigations confirmed AL amyloidosis with multi-organ involvement (liver, kidneys, heart).
Progression and Readmission
Clinical Course
The patient was discharged after stabilization but was readmitted one month later with:
- Worsening ascites
- New-onset jaundice
This led to repeat laboratory testing and liver function tests.
Liver Function Tests on Readmission
- Total Bilirubin: 21.6 mg/dL (significant increase)
- Alkaline Phosphatase (AP): 1317 IU/L (severe rise)
- AST: 260 IU/L (continued rise)
- ALT: 104 IU/L (persistently raised)
Clinical Interpretation of Results
1. Total Bilirubin – 21.6 mg/dL
- Inhibits severe cholestasis and hepatic dysfunction.
- Jaundice becomes clinically apparent once bilirubin >2–3 mg/dL; at >20 mg/dL, prognosis is very bad.
- Indicates extensive amyloid infiltration of hepatic tissue, causing bile excretion to be impaired.
2. Alkaline Phosphatase (AP) – 1317 IU/L
- Represents cholestatic pattern of liver damage.
- Considerable elevation is characteristic of hepatic amyloidosis, in which amyloid fibrils invade the biliary canalicular system.
3. AST – 260 IU/L
- Raised, indicative of hepatocellular damage.
- In amyloidosis, AST can be increased due to compression of hepatocytes and ischemic damage from infiltrative disease.
4. ALT – 104 IU/L
- Mild-moderate elevation, frequently less than AST in amyloidosis.
- Indicates persistent hepatocellular stress but not the etiology of dysfunction.
Pathophysiology of Hepatic Amyloidosis
Amyloid fibrils accumulate in liver parenchyma, portal tracts, and sinusoids. This results in:
- Cholestasis → obstructed bile flow, hyperbilirubinemia
- Portal hypertension → ascites, splenomegaly (although missing in this case)
- Hepatomegaly (sometimes, not always)
- Progressive hepatic failure
The lab profile (wickedly elevated bilirubin, elevated AP, moderate AST/ALT) is 典型的advanced hepatic amyloidosis.
Clinical Implications of Severe Liver Dysfunction
- Prognosis
- Severe hyperbilirubinemia in amyloidosis is linked with median survival of less than 6 months.
- Bilirubin elevation >10 mg/dL shortens survival dramatically after that.
- Treatment Difficulty
- Bilirubin has a narrow window for systemic chemotherapy (e.g., bortezomib, cyclophosphamide, dexamethasone) eligibility.
- Supportive care becomes the norm.
- Complications Likely
- Hepatic encephalopathy
- Coagulopathy (dysfunctional INR, risk of bleeding)
- Spontaneous bacterial peritonitis (recurring ascites)
- Progressive renal failure (hepatorenal syndrome)
Management Strategies
Supportive Therapy
- Large-volume paracentesis for relief of ascites
- Albumin infusion to maintain oncotic pressure
- Diuretics (spironolactone/furosemide) used cautiously
- Nutritional support with high-protein diet (as tolerated)
Systemic Treatment
- Systemic treatments are not tolerated in advanced liver dysfunction.
- High-risk regimens and clinical trials may not be viable.
Palliative Care
- Symptom management takes center stage.
- Quality of life talks with the family are critical.
Literature Insights
- Kyle RA & Gertz MA: Patients with jaundice and elevated bilirubin in hepatic amyloidosis generally have survival in weeks to months.
- Falk RH: Involvement of the liver is prognostic for worse systemic outcome, particularly if bilirubin >20 mg/dL.
- Case reports in the medical literature highlight that once bilirubin is more than 15–20 mg/dL, systemic therapy is hardly an option.
Key Learning Points
- Rapid progression: Amyloidosis can deteriorate rapidly in weeks.
- Lab pattern recognition: Elevated bilirubin + elevated AP + moderate AST/ALT is characteristic of hepatic amyloidosis.
- Prognostic marker: Bilirubin >20 mg/dL is a bad prognostic indicator.
- Treatment limitations: Advanced hepatic failure limits systemic therapy options.
- Early detection is necessary: Early diagnosis enables the initiation of amyloidosis-directed treatments prior to hepatic decompensation.
Conclusion
In this case of a 61-year-old patient presenting with AL amyloidosis, the catastrophizing course of hepatic involvement is seen, ending in severe liver dysfunction with a bilirubin level of 21.6 mg/dL, accompanied by extremely high AP, AST, and ALT levels.
The case reemphasizes that:
- Liver involvement is a late and ominous sign in amyloidosis.
- After severe jaundice appears, prognosis is not good and there are recommendations but no treatment.
- Attention is directed toward relief of symptoms, supportive measures, and maintaining quality of life.
This document contributes to the increasing evidence that early detection and management of amyloidosis are essential prior to developing irreversible hepatic failure.

