Case Report: Liver Biopsy Confirming Amyloidosis Without Inflammation, Fibrosis, or Malignancy in a 61-Year-Old Patient
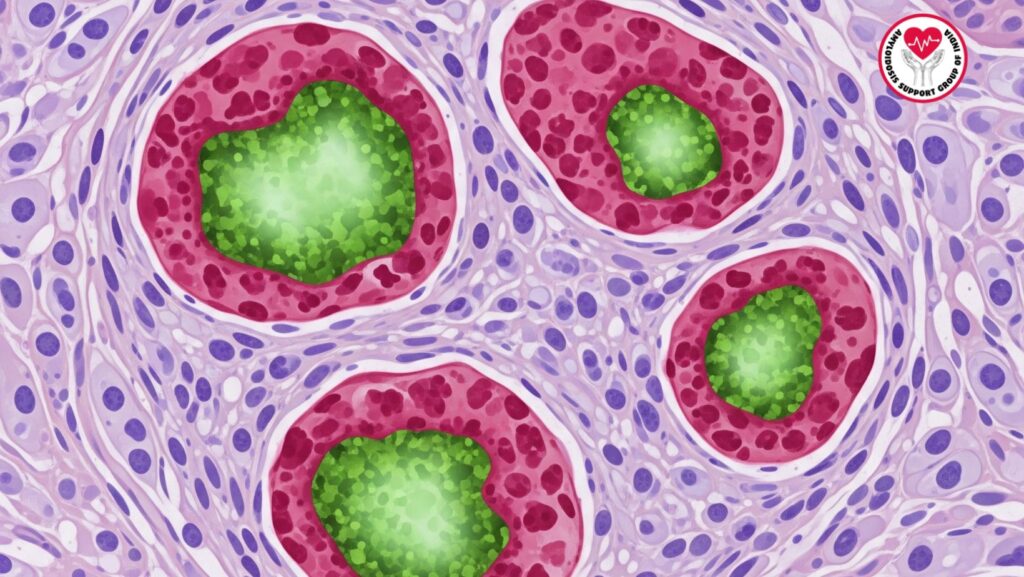
Table of Contents
Introduction
Amyloidosis is a multisystem, complex disease due to extracellular deposition of abnormally folded amyloid fibrils. Hepatic presentation of amyloidosis tends to be under-diagnosed, presenting with overlapping symptoms of other liver conditions like cirrhosis, hepatitis, or malignancy. This case report describes the clinical course of a 61-year-old patient whose liver biopsy was diagnosed with amyloidosis without inflammation, fibrosis, or malignancy, illustrating diagnostic pitfalls and important clinical pearls.
In this article, we discuss:
- The clinical presentation and history of the patient
- Imaging and laboratory results
- Histopathological findings and details of liver biopsy
- Role of biopsy in amyloidosis diagnosis
- Significance of the lack of inflammation, fibrosis, or malignancy
- Prognosis and management strategies
- Implications for hepatic amyloidosis care and diagnosis at large
Patient Background and Initial Presentation
The patient, a 61-year-old man, first came in with progressive abdominal distension and bilateral lower extremity swelling. During the course of his clinical history taking, several laboratory and imaging investigations suspected underlying hepatic impairment. Over the period of time, his condition progressively got worse to the point of readmission with jaundice as well as severe biochemical derangements.
Most Important Symptoms Described
- Subacute abdominal distension secondary to ascites
- Bilateral pedal edema (progressively increasing in severity)
- Early satiety and fatigue
- Deteriorating jaundice at readmission
Laboratory and Imaging Findings
Baseline Investigations
- Albumin: 2.1 g/dL (hypoalbuminemia)
- Liver Enzymes: Alkaline phosphatase elevated (AP 718 IU/L), AST 158 IU/L, ALT 119 IU/L
- Total Bilirubin: Initially within normal limits (0.5 mg/dL) but later rose exponentially to 21.6 mg/dL at readmission
- Creatinine: 0.9 mg/dL (renal function was normal initially)
- Coagulation: INR 1.07
Ascitic Fluid Analysis
- Serum Ascites Albumin Gradient (SAAG): >1.1, which is indicative of portal hypertension
- Negative for malignant cells or infection
Imaging Tests
- Abdominal CT scan: Ascites, potentially nodular liver, hepatosplenomegaly absent
- Transthoracic echocardiogram: Left ventricular hypertrophy suspicious for infiltrative disease
Liver Biopsy Procedure
Due to the patient’s severe hepatic impairment and risk of coagulopathy, a transjugular liver biopsy was done during readmission. This method is frequently employed in high-risk patients because it minimizes the risk of bleeding complications yet provides sufficient tissue sampling.
Histopathology Results
- Amyloid deposits verified by Congo red staining with apple-green birefringence under polarized light
- There was no significant inflammation
- No fibrosis or cirrhosis
- No malignancy or granulomas
Clinical Relevance of Biopsy Results
1. Confirmation of Amyloidosis
The biopsy conclusively confirmed hepatic amyloidosis as the etiology of the patient’s liver impairment.
2. Lack of Inflammation
In contrast to autoimmune or infectious hepatitis, inflammatory activity was absent, further attesting that the pathology was secondary to protein deposition and not immune-mediated damage.
3. No Fibrosis or Malignancy
This excluded cirrhosis and hepatic malignancies like hepatocellular carcinoma, which may have overlapping biochemical and imaging features.
4. Primary AL Amyloidosis
Mass spectrometry conducted previously established a peptide pattern compatible with primary (AL) amyloidosis, endorsing the systemic nature of the disease.
Management Considerations
Supportive Care
- Diuretics for ascites management
- Nutritional support with high-protein diet
- Salt restriction to control edema
Targeted Therapy
- Chemotherapy-based regimens (bortezomib, cyclophosphamide, dexamethasone) are usually employed in AL amyloidosis for the purpose of decreasing light-chain production.
- Consideration of autologous stem cell transplantation in eligible patients.
Prognosis
Hepatic amyloidosis is associated with a poor prognosis, particularly if the bilirubin level increases significantly. In the absence of fibrosis or cirrhosis, there is an implication of early structural integrity, but severe biochemical worsening remains the key risk factor.
Broader Insights into Hepatic Amyloidosis
- Diagnostic Challenges Most patients with hepatic amyloidosis are initially diagnosed as having cirrhosis, cholestatic liver disease, or malignancy before amyloid deposition is established on biopsy.
- **Role of Non-Invasive Imaging
While imaging may suggest hepatomegaly and nodularity, it cannot be used to differentiate amyloidosis from other causes reliably.
- Multidisciplinary Care
Hepatologists, hematologists, and pathologists need to work together to guarantee prompt diagnosis and initiation of treatment.
Conclusion
This case highlights the diagnostic relevance of amyloidosis liver biopsy, especially in those patients who have unexplained hepatic failure. The diagnosis of amyloidosis in the absence of inflammation, fibrosis, or malignancy underscores the specificity of this disease and its potential to masquerade other liver diseases.
For clinicians, this case points to the importance of early recognition, proper diagnosis, and timely multidisciplinary intervention. For patients and families, it underscores the necessity of specialist care for rare diseases such as hepatic amyloidosis.

