Clinical Presentation of Liver Involvement in AL Amyloidosis – Silent Development, Minor LFT Abnormalities, and Hepatomegaly
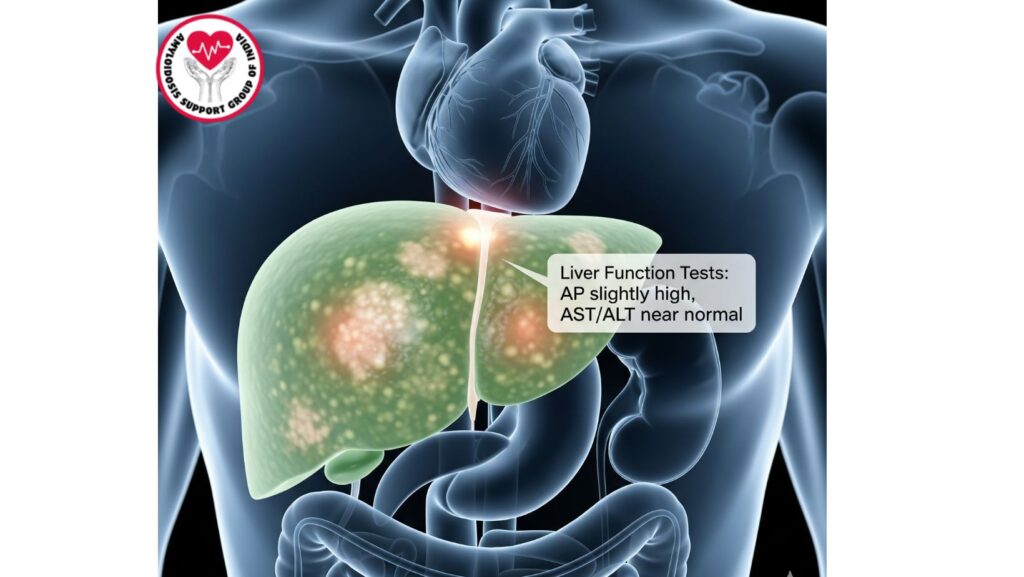
Table of Contents
Introduction
Systemic primary amyloidosis (AL amyloidosis) is an uncommon condition resulting from the deposition of light chain immunoglobulin misfolding in organs. The liver is commonly affected, with 60–90% of patients demonstrating some hepatic infiltration. Notwithstanding its frequency, liver involvement is usually clinically silent, and a majority of patients have only minimal abnormalities in liver function tests (LFTs) or hepatomegaly.
Identifying these subtle clinical presentations is important because early diagnosis facilitates improved monitoring, management, and prognosis evaluation. This article reviews the clinical presentations, pathophysiology, diagnosis, and implications of liver involvement in AL amyloidosis.
Epidemiology of Hepatic Amyloidosis
- Prevalence: Hepatic involvement in 60–90% of systemic AL amyloidosis cases.
- Age: Patients most commonly present at 50–70 years of age.
- Gender: Mild male predominance has been reported in several case series.
- Risk Factors:
- Underlying plasma cell disorders that produce monoclonal light chains
- Multiorgan involvement with heart, kidney, and gastrointestinal tract
Pathophysiology
Amyloid deposition in the liver mainly occurs in:
- Sinusoids: Amyloid fibrils deposit in the space of Disse, which impairs hepatocyte function.
- Portal tracts: Causes mild compression of hepatocytes and cholestatic changes.
- Vascular walls: May compromise hepatic blood flow and cause portal hypertension in late stages.
Mechanisms Contributing to Silent Disease
- Subclinical hepatocyte compression enables liver function to be well-maintained initially.
- Mild biochemical abnormalities in LFTs can go undetected.
- Gradual progression results in patients presenting minimally until advanced stages or multi-organ impairment sets in.
Clinical Features
Silent or Subclinical Presentation
- Most patients are asymptomatic with hepatic involvement identified incidentally on imaging or biopsy.
- Physical examination may detect hepatomegaly, typically without tenderness.
Mild Liver Function Test Abnormalities
- Alkaline phosphatase (AP): Most frequently elevated enzyme.
- AST/ALT: Mild elevations in a minority of patients.
- Bilirubin: Typically normal; marked elevation is a sign of advanced disease.
- Albumin: Decreases if concomitant nephrotic syndrome exists.
Hepatomegaly
- Painless hepatomegaly is characteristic of liver involvement.
- Typically discovered on routine physical examination or imaging.
- Severe hepatomegaly occurs infrequently and signifies advanced infiltration.
Less Frequent Manifestations
- Cholestasis: Benign, infrequently symptomatic.
- Ascites: Usually develops in late disease, most frequently with hypoalbuminemia or portal hypertension.
- Fatigue and anorexia: Non-specific, frequently a result of systemic disease more than hepatic disease per se.
Diagnostic Evaluation
Laboratory Investigations
- Liver function tests (LFTs): Most sensitive to mild AP elevation.
- Serum protein electrophoresis (SPEP)/urine protein electrophoresis (UPEP): Identify monoclonal light chains.
- Serum free light chain assay: Quantitates amyloidogenic proteins for monitoring.
Imaging
- Ultrasound: Identifies hepatomegaly, occasionally heterogeneous echotexture.
- CT/MRI: May demonstrate nodular liver appearance; helpful in distinguishing amyloidosis from other infiltrative diseases.
Liver Biopsy
- Gold standard for confirmation: Congo red staining demonstrates apple-green birefringence under polarized light.
- Mass spectrometry: Validates AL amyloidosis subtype.
- Transjugular approach: Advised in coagulopathy, ascites, or portal hypertension patients.
Prognostic Implications
*
- Isolated liver involvement infrequently leads to mortality.
- Combined organ involvement (heart, kidney) deteriorates prognosis.
- Markers of advanced hepatic disease:
- Jaundice
- Ascites
- Portal hypertension
- MELD score: May be utilized to assess liver reserve in advanced disease.
Management Strategies
*
Medical Management
- Plasma cell–directed therapy: Bortezomib, cyclophosphamide, dexamethasone, or daratumumab.
- Supportive care:
- Diuretics for ascites
- Nutritional support
- Symptom monitoring
Advanced Interventions
- Liver transplantation: Used very infrequently, primarily in single-organ hepatic amyloidosis.
- Combined organ transplantation: Reserved for individual cases with multi-organ disease.
Emerging Therapies
- Amyloid fibril stabilizers – being explored.
- RNA-silencing therapies – mostly in hereditary amyloidosis but with possible applicability to AL types.
- Monoclonal antibodies against amyloid deposits – ongoing clinical trials.
Case Examples from Literature
- Incidental hepatomegaly: Patient identified incidentally on routine imaging; modest elevation of AP; treated with bortezomib with response.
- Symptomatic liver disease: Patient with ascites and fatigue; amyloidosis confirmed by liver biopsy; systemic treatment initiated with partial remission.
- Advanced multi-organ disease: Involvement of the liver identified with hepatomegaly; patient eventually went to palliative care with cardiac and renal failure.
Clinical Pearls
- Silent course is the characteristic of hepatic AL amyloidosis.
- Subtle LFT derangements must be suspected, especially in those with established AL amyloidosis or plasma cell disease.
- Hepatomegaly is the most frequent physical examination finding.
- Multidisciplinary management (hepatology, hematology, cardiology) is optimal for treatment.
- Early diagnosis enables appropriate systemic therapy and enhances quality of life.
Future Directions
*
- Biomarker discovery for early liver involvement detection.
- New therapies against liver amyloid deposits.
- Palliative care integration in end-stage multi-organ disease.
- Transplantation trials in sporadic hepatic amyloidosis.
Conclusion
Liver involvement in AL amyloidosis is common but frequently clinically occult, with a presentation of midliver function test aberrations and hepatomegaly. Although isolated liver disease infrequently influences prognosis, hepatic involvement awareness is essential for:
- Systemic disease monitoring
- Informing therapeutic decisions
- Enhancing patient quality of life
Early diagnosis, multidisciplinary treatment, and individualized therapy are key to best results in patients with AL amyloidosis involving the liver.

