Influence of Liver Failure on Treatment in AL Amyloidosis – Challenges and Clinical Considerations
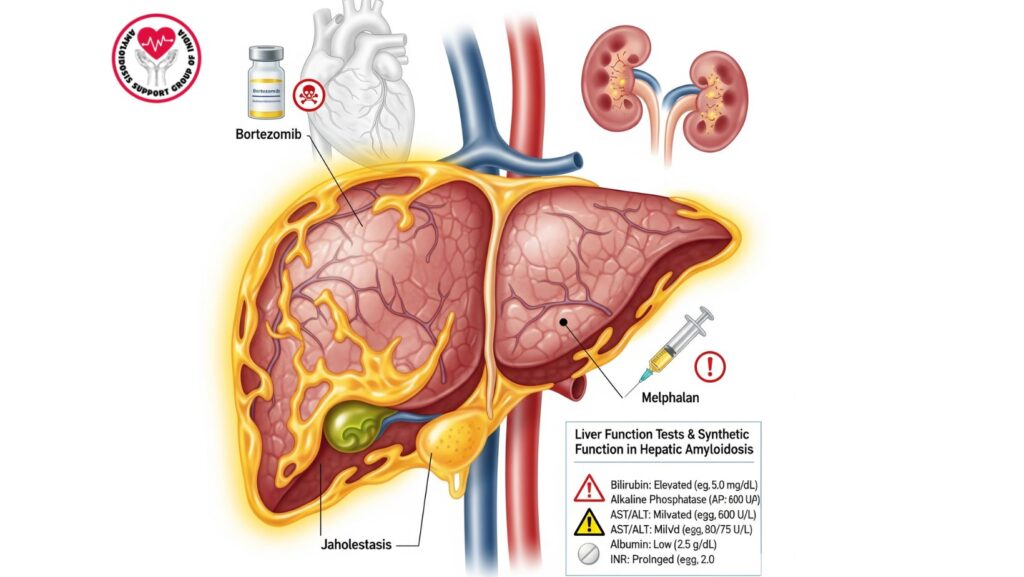
Table of Contents
Introduction
Primary (AL) amyloidosis is a uncommon condition resulting from misfolded immunoglobulin light chains that accumulate as amyloid fibrils in various organs, such as the heart, kidneys, and liver. Although the liver is affected in 60–90% of cases, the majority of patients present with mild, clinically occult disease.
Yet, severe liver impairment or liver failure constitutes a serious therapeutic problem. Normal modalities of treatment for AL amyloidosis, like bortezomib, melphalan, and other chemotherapeutic agents, are hepatically metabolized. Liver impairment may compromise drug clearance, enhance the risk of toxicity, and constrain therapeutic choice, especially in patients with cholestatic liver failure or jaundice.
This article discusses:
- The effect of liver failure on therapy in AL amyloidosis
- Pharmacokinetics in drugs most frequently employed in hepatic impairment
- Supportive care and clinical management strategies
- Alternative approaches and future directions
Epidemiology of Liver Involvement in AL Amyloidosis
- Liver involvement affects 60–90% of patients with systemic AL amyloidosis.
- Severe cholestatic liver failure is unusual (~5–10% of cases of hepatic involvement).
- Multi-organ involvement, particularly cardiac and renal, complicates therapy and worsens prognosis.
Pathophysiology of Liver Dysfunction
Mechanisms of Hepatic Impairment in AL Amyloidosis
- Sinusoidal amyloid deposition – impairs hepatocyte function and bile drainage.
- Portal tract infiltration – leads to cholestasis.
- Vascular compromise – lowers hepatic perfusion.
- Combined multi-organ dysfunction – exacerbates drug metabolism and elimination.
Effects of Liver Failure
- Defective drug metabolism due to decreased cytochrome P450 activity.
- Abnormal plasma protein binding impacts drug distribution.
- Elevated risk of toxicity from conventional chemotherapy schedules.
- Impaired synthetic function: hypoalbuminemia, coagulopathy, and ascites.
Impact on Treatment Options
Bortezomib
- Mainly metabolized by the liver (cytochrome P450 3A4 and 2C19).
- Liver failure may cause drug accumulation and enhanced risk of neuropathy, cytopenias, and hepatotoxicity.
- Dose adjustment needed in hepatic impairment patients.
Melphalan
- Metabolized and renally excreted by the liver.
- Liver impairment may enhance systemic toxicity, such as myelosuppression and mucositis.
- Usually contraindicated in severe hepatic failure.
Other Chemotherapeutic Agents
- Cyclophosphamide: Dose adjustment in liver impairment.
- Daratumumab: Less hepatotoxic but caution may still be necessary with severe liver failure.
- Thalidomide/Lenalidomide: Minimal metabolism by the liver; safer options in appropriate patients.
Clinical Considerations
Patient Assessment
- Liver function tests: AST, ALT, ALP, bilirubin, albumin, INR
- Extent of liver involvement: Imaging (ultrasound, CT, MRI)
- Multi-organ involvement: Cardiac, renal, and gastrointestinal systems
Risk Stratification
- Patients with jaundice, elevated bilirubin, or synthetic failure are at greatest risk for complications related to therapy.
- Consider supportive therapy or palliative care when conventional treatments are contraindicated.
Dose Modifications and Monitoring
- Decreased or altered dosing of drugs metabolized by the liver
- Vigilant monitoring of coagulation parameters and LFTs
- Regular monitoring for adverse effects and toxicity
Alternative Approaches to Management
Supportive Management
- Hypoalbuminemia treatment with nutritional support
- Paracentesis and diuretics for ascites
- Symptom control for pruritus and fatigue
Palliative Care
- Directed at quality of life in multi-organ amyloidosis and end-stage liver failure patients
- Early integration proposed in rapidly progressive cholestatic liver disease
Investigational Therapies
- New agents for targeting amyloid deposits
- Therapies that are less hepatically dependent for their metabolism
- Clinical trials to test safe regimens for hepatic impairment
Case Studies
- Patient A: Extensive cholestatic liver failure; reduced dose of bortezomib secondary to hepatic impairment. Developed neuropathy, needed therapy adjustment.
- Patient B: Multi-organ AL amyloidosis with high bilirubin; melphalan was avoided due to risk of toxicity; supportive and palliative care were given priority.
- Patient C: Isolated hepatic amyloidosis; thalidomide-based regimen was given safely with careful follow-up of liver function.
Clinical Pearls
- Liver failure restricts conventional chemotherapy because of compromised drug metabolism and potential for increased toxicity.
- Adjustment of dosage and meticulous monitoring are paramount in utilizing hepatically metabolized agents.
- Other therapies and supportive care might be indicated in patients with advanced hepatic impairment.
- Recognition of liver involvement as soon as possible is crucial for therapeutic planning and patient safety.
Future Directions
- Creation of hepatic-sparing therapies for AL amyloidosis
- Biomarkers for risk stratification of patients at high risk of liver-related toxicity
- Clinical trials on safe chemotherapy regimens in advanced hepatic impairment
- Examination of liver-directed therapies or combination strategies to decrease systemic amyloid burden
Conclusion
Liver failure in AL amyloidosis presents formidable challenges to treatment, especially for agents such as bortezomib and melphalan that are subjected to hepatic metabolism. Main points:
- Hepatic impairment with increased risk of toxicity and complications.
- Dose adjustments or other therapies might be needed.
- Symptomatic and palliative care are the main role when optimal treatment is not feasible.
- Multidisciplinary treatment is necessary to maximize safety, efficacy, and quality of life.
Knowledge of the effect of hepatic dysfunction on therapy is crucial in clinicians treating AL amyloidosis patients with hepatic involvement.

