Why Liver Transplantation Was Not an Option: Multi-Organ Involvement in AL Amyloidosis
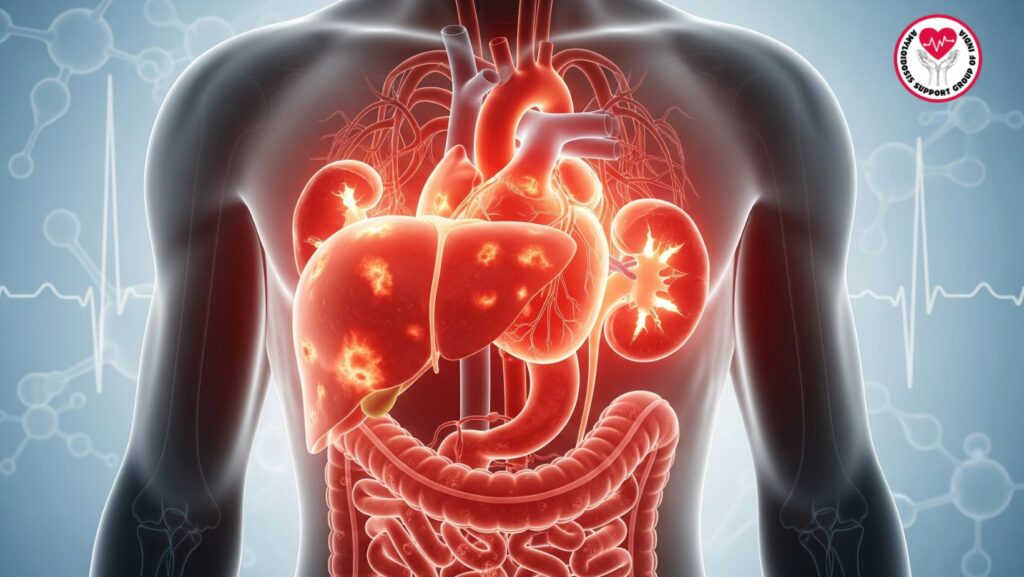
Table of Contents
Introduction
Amyloidosis is an uncommon but debilitating disease due to the accumulation of abnormal amyloid fibrils in many organs. Of the various forms, primary systemic amyloidosis (AL type) is most commonly linked with plasma cell dyscrasias and can affect multiple organs, including the heart, kidneys, gastrointestinal tract, and liver.
In patients with hepatic amyloidosis, threatened liver failure is an indication for raising the question of liver transplantation. Yet, in contrast to non-contagious liver diseases like cirrhosis or viral hepatitis, multi-organ involvement in amyloidosis considerably hampers the decision. This paper discusses at length why liver transplantation is usually not indicated in severe systemic amyloidosis and why multi-organ amyloidosis affects prognosis and therapeutic approach.
1. Understanding AL Amyloidosis
- Definition of AL amyloidosis.
- Misfolding of monoclonal light chains and deposition as amyloid fibrils.
- Systemic vs. localized amyloidosis.
- Organs most frequently involved: kidneys (proteinuria, nephrotic syndrome), heart (restrictive cardiomyopathy), liver (hepatomegaly, cholestasis), and nervous system (neuropathy).
2. Liver Involvement in AL Amyloidosis
- Pathophysiology of amyloid deposition in hepatic sinusoids and vessels.
- Clinical manifestations: hepatomegaly, mild alkaline phosphatase elevation, hypoalbuminemia, ascites.
- Uncommon presentation: profound cholestatic liver failure and jaundice.
- Diagnostic processes: LFTs, imaging, biopsy with Congo red stain, mass spectrometry confirmation.
3. Liver Transplantation Role in General
- Indications of liver transplant for chronic liver disease.
- MELD score and patient prioritization.
- Success experiences with viral hepatitis, alcoholic liver disease, autoimmune hepatitis.
- Why transplantation is a curative approach to most end-stage liver diseases.
4. Why Liver Transplantation Is Controversial in Amyloidosis
- AL amyloidosis is not localized to the liver.
- Even with replacement of the liver, other organs (heart, kidneys) are still involved.
- Transplant does not interrupt production of amyloidogenic light chains.
- High risk of recurrence in the transplanted liver.
- Immunosuppression after transplant could worsen systemic progression.
5. Multi-Organ Involvement: The Critical Barrier
- Cardiac involvement: restrictive cardiomyopathy, arrhythmias, poor surgical tolerance.
- Kidney involvement: nephrotic syndrome, progressive renal failure.
- Nervous system involvement: autonomic dysfunction causing perioperative instability.
- Prognosis is mainly determined by cardiac amyloidosis and not hepatic disease.
6. Case Discussion: Why This Patient Was Not Eligible
- 61-year-old patient with AL amyloidosis.
- Hepatic involvement: progressive jaundice, cholestasis, ascites.
- Cardiac findings: left ventricular hypertrophy indicating infiltrative disease.
- Renal function deterioration: worsening creatinine, nephrotic-range proteinuria.
- Multi-organ amyloidosis precluded a liver transplant from enhancing overall survival.
- Transplantation was not done by the clinical team and supportive care was initiated.
7. Prognosis in Hepatic Amyloidosis
- In the absence of jaundice: median survival ~2 years.
- With jaundice: median survival ~3 months.
- The prognostic significance of cardiac involvement.
- Constraints of supportive treatment.
8. Systemic Therapy vs. Transplantation
- The role of chemotherapy (melphalan, bortezomib, dexamethasone).
- Autologous stem cell transplantation (ASCT) as a choice in carefully selected patients.
- Why systemic therapy targets the root cause (light chain production), as opposed to liver transplant.
- Clinical trials in progress that target amyloid fibril clearance.
9. Clinical Guidelines and Transplant Eligibility
- American Association for the Study of Liver Diseases (AASLD) criteria.
- European guidelines for amyloidosis and liver transplantation.
- Why isolated organ transplant is seldom advised in systemic AL amyloidosis.
- Planning for combined liver-kidney or heart-liver transplant only in highly selected situations.
10. Ethical and Clinical Considerations
- Weighing limited organ availability against realistic expectations.
- Early recurrence risk and poor prognosis curtailing transplant benefit.
- Palliative care discussions becoming important.
11. Future Directions
- Novel therapies decreasing amyloidogenic light chains earlier in disease.
- Investigating fibril-targeted treatments (monoclonal antibodies, doxycycline, tauroursodeoxycholic acid).
- Gene-editing and plasma cell–targeted strategies.
- Optimism for broadening transplant possibilities if systemic control increases.
12. Key Takeaways
- Liver transplantation is not viable in the majority of AL amyloidosis due to multi-organ involvement.
- Transplant does not treat systemic amyloid deposition or light-chain production.
- Prognosis is more based on cardiac involvement than liver disease itself.
- Systemic therapy and supportive care are still the major management strategies.
Conclusion
In systemic AL amyloidosis, liver involvement is common, but transplantation is not curative in the case of multi-organ involvement. This case illustrates the grim truth that amyloid deposition in multiple organs excludes transplant candidacy. For physicians, prompt identification of amyloidosis in patients with unexplained liver disease is paramount, but therapy needs to concentrate on systemic treatment, not organ replacement.

