How Amyloid Deposition Causes Liver Dysfunction: Causes, Symptoms, and Management
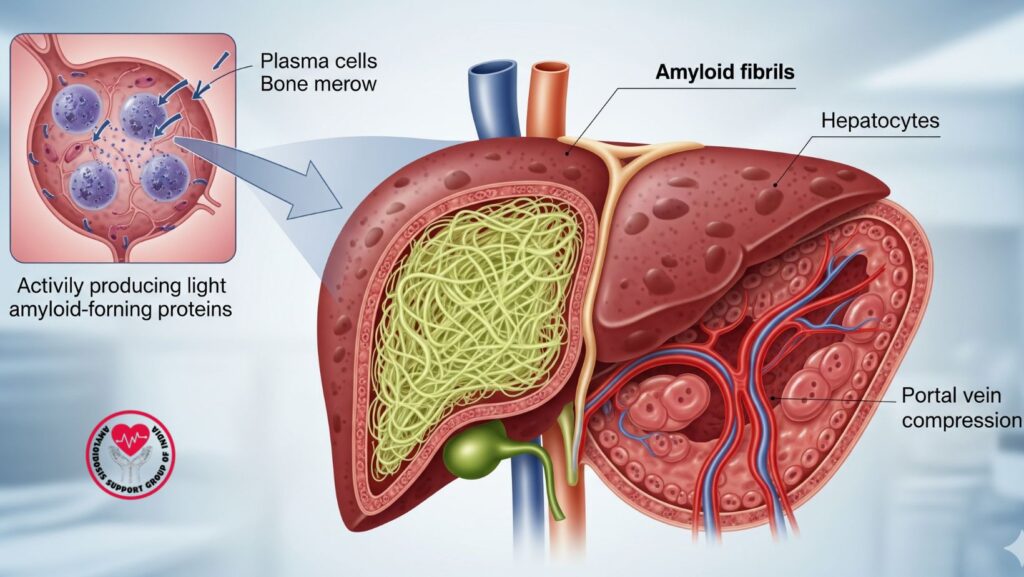
Table of Contents
1. Introduction
Amyloidosis is an uncommon but dangerous condition resulting from the abnormal deposition of amyloid proteins in tissues and organs. When amyloid proteins deposit in the liver, they cause interference with the normal structure and function, and most commonly lead to liver dysfunction and ultimately fatal complications.
Liver involvement is frequent in AL (light chain) amyloidosis, but can also happen in AA and ATTR types. Patients can have nonspecific symptoms early on, which can postpone diagnosis and treatment.
Knowing how amyloid deposition impacts the liver, the detection of early signs, and the introduction of timely treatment are paramount to enhancing outcome. This article discusses the causes, symptoms, diagnosis, treatment, and supportive measures for effective treatment of liver amyloidosis.
2. Understanding Amyloid Deposition
What Are Amyloid Proteins?
Amyloid proteins are misfolded proteins that create insoluble fibrils in tissues. Unlike regular proteins, these fibrils cannot be degraded by the body, resulting in progressive organ failure.
How Misfolded Proteins Build Up
- Abnormal plasma cells (in AL amyloidosis) secrete excess light chains.
- Chains misfold and clump into amyloid fibrils.
- Fibrils accumulate in the liver, squishing hepatocytes and blood vessels.
Types of Amyloidosis That Involve the Liver
- AL (Primary) Amyloidosis: Most prevalent; due to plasma cell disorders.
- AA (Secondary) Amyloidosis: With chronic inflammation or infections.
- ATTR Amyloidosis: Due to transthyretin protein deposits; less frequent in the liver.
These deposits gradually worsen liver function, frequently prior to symptom development.
3. Pathophysiology of Liver Dysfunction in Amyloidosis
Amyloid deposition in the liver leads to dysfunction by a number of mechanisms:
- Structural Disruption: Fibrils invade liver tissue, pushing hepatocytes apart and disrupting normal architecture.
- Vascular Compression: Amyloid deposits constrict blood vessels, impairing hepatic blood flow.
- Impaired Protein Synthesis: Hepatocytes synthesize fewer proteins such as albumin and clotting factors.
- Progressive Fibrosis: Chronic deposition can cause fibrosis, portal hypertension, and ultimately liver failure.
The liver’s inherent resilience tends to conceal early dysfunction, and that is why regular monitoring is crucial for at-risk patients.
4. Symptoms of Liver Amyloidosis
Involvement of the liver is subtly present at first. The usual symptoms are:
Early-Stage Symptoms
- Slight hepatomegaly (enlarged liver)
- Fatigue
- Slight abdominal pain
Advanced-Stage Symptoms
- Jaundice (yellowing of eyes and skin)
- Ascites (fluid in the abdomen)
- Easy bruising or bleeding
- Severe weakness and fatigue
Laboratory Indicators
- Increased alkaline phosphatase (ALP)
- Slightly raised bilirubin
- Low albumin in advanced disease
- Coagulopathy due to altered clotting factor production
Knowing these signs early enhances the possibility of timely intervention.
. 5. Diagnostic Methods
Proper diagnosis depends on a combination of tests:
Blood Tests
- Liver function tests (ALT, AST, ALP, bilirubin)
- Serum albumin and total protein
- Serum free light chain assay (for AL amyloidosis)
Imaging
- Ultrasound: Hyperechoic liver with enlarged size
- CT/MRI: Structural changes and infiltration patterns are detected
- Elastography: Quantifies liver stiffness for fibrosis
Biopsy
- Gold standard: Liver biopsy under Congo red staining demonstrates apple-green birefringence upon polarized light.
- Verifies type of amyloid protein and degree of infiltration.
New Tools
- PET-CT and new biomarkers for non-invasive diagnosis.
6. Effect of Amyloid Deposition on Liver Function
Amyloid infiltration affects various liver functions:
- Production of Proteins: Decreased albumin causes edema; decreased clotting factors result in bleeding.
- Bile Production & Excretion: Cholestasis may follow, leading to jaundice and pruritus.
- Portal Hypertension: Hepatic blood flow compression increases pressure in the portal vein, which causes ascites and varices.
- Risk of Liver Failure: Extensive deposition can lead to end-stage liver disease.
Multi-organ involvement usually makes treatment complicated and multidisciplinary.
7. Treatment Strategies for Liver Amyloidosis
Treatment is intended to curb amyloid production, eliminate deposits, and treat complications.
Targeting Underlying Amyloidosis
- AL type: Chemotherapy, proteasome inhibitors (bortezomib), melphalan, stem cell transplantation.
- AA type: Address underlying inflammatory condition (e.g., rheumatoid arthritis, chronic infection).
- ATTR type: Tafamidis or patisiran to stabilize or decrease transthyretin deposits.
Symptomatic Treatment
- Diuretics for fluid overload
- Liver-protective drugs
- Control of coagulopathy
Advanced Interventions
- Stem Cell Transplantation: Reserved in healthy AL patients for long-term remission.
- Liver Transplant: In exceptional cases of isolated liver failure.
Treatment needs to be individualized according to type of amyloidosis, liver involvement, and comorbidities.
8. Lifestyle and Supportive Care
Lifestyle changes by the patient are essential:
- Diet: Increased protein, low salt to prevent fluid buildup.
- Avoidance of hepatotoxins: Restrict alcohol and some medications.
- Monitoring: Serial liver function tests and imaging.
- Supportive therapy: Gentle exercise, stress reduction, and patient support groups.
Supportive care enhances quality of life and optimizes the delivery of disease-directed treatments.
9. Case Studies and Clinical Evidence
Example 1: AL Amyloidosis
- 58-year-old patient presenting with fatigue and hepatomegaly.
- Liver biopsy revealed AL amyloid deposits.
- Treated with bortezomib + dexamethasone → normalization of liver function within 6 months.
Example 2: AA Amyloidosis
- Chronic rheumatoid arthritis in a 65-year-old patient developed jaundice.
- Management of inflammation + colchicine therapy lowered levels of liver enzymes.
These examples point out the necessity of earlier diagnosis and targeted treatment.
10. Emerging Therapies and Research
Emerging therapies are:
- Monoclonal antibodies (CAEL-101, daratumumab): Act on amyloid fibrils directly.
- Gene silencing therapy: In ATTR amyloidosis to decrease transthyretin production.
- Clinical trials: Examining combination therapies to enhance liver function and survival.
Studies are progressing fast, providing better long-term outlooks.
11. Complications and Prognosis
- Poor prognosis risk factors: Old age, multi-organ involvement, late diagnosis.
- Possible complications: Liver failure, portal hypertension, ascites, variceal bleeding.
- Prognosis is better with early diagnosis, targeted therapy, and follow-up.
12. Coping Strategies and Patient Awareness
- Educate oneself about early symptoms: fatigue, abdominal pain, jaundice.
- Obtain specialist care from amyloidosis centers.
- Participate in support networks such as amyloidosissupport.in.
- Utilize mental health support to deal with chronic disease.
13. Conclusion
Deposition of amyloid in the liver can cause severe dysfunction, but early diagnosis, targeted treatment, and support care can radically alter outcomes.
Key takeaways:
- Identify early liver involvement in amyloidosis.
- Employ a combination of diagnostic tools for proper detection.
- Treat underlying amyloidosis while treating liver symptoms.
- Be updated on emerging therapies and research for optimism and quality of life.

