Clinical Implication of Normal Total Bilirubin in Liver Disease: Early Maintenance of Function
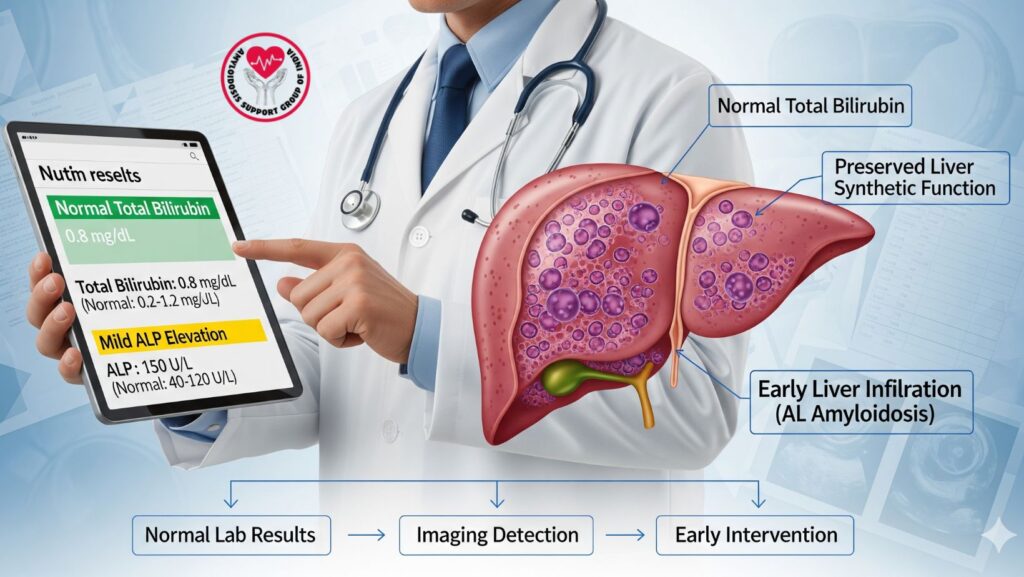
Table of Contents
Introduction
Liver disease may be subtle, and early laboratory results are paramount in recognizing subclinical organ dysfunction. Total bilirubin, one of the most important indicators of liver function, will frequently remain normal despite the presence of other abnormalities.
Knowledge of the clinical implication of a normal total bilirubin aids clinicians:
- In assessment of liver synthetic function
- In identifying disease stage
- Identify patients who may benefit from early intervention
- Distinguish between hepatic and non-hepatic causes of laboratory abnormalities
This article explores the significance of normal bilirubin, laboratory correlations, clinical interpretation, and implications for early liver disease detection, with a focus on infiltrative disorders like amyloidosis.
1. Understanding Total Bilirubin
Bilirubin is a yellow pigment formed from heme breakdown in red blood cells. It exists in two forms:
- Unconjugated (indirect) bilirubin: Formed in the spleen and delivered to the liver.
- Conjugated (direct) bilirubin: Metabolized by the liver and eliminated through bile.
Total bilirubin quantifies the sum of direct and indirect bilirubin in serum.
Normal Reference Range
- Adults: 0.3–1.2 mg/dL (may differ slightly by lab)
2. Liver Function and Bilirubin
Bilirubin levels are a reflection of liver synthetic and excretory function:
- Normal total bilirubin: Indicates intact hepatocyte function and bile excretion.
- Raised bilirubin: Suggests hepatocellular damage, bile duct obstruction, or hemolysis.
In subclinical or initial liver disease, bilirubin is usually normal, whereas other markers, such as alkaline phosphatase (ALP) or AST/ALT, can be abnormal.
3. Relevance of Normal Bilirubin to Clinical Practice
3.1 Maintenance of Liver Synthesis Function
- Normal total bilirubin means that hepatocytes are working properly, despite the presence of structural or infiltrative pathology.
- Patients can have other laboratory abnormalities (e.g., mild ALP elevation, proteinuria in amyloidosis) without jaundice.
3.2 Early Detection Window
- Normal bilirubin can delay symptom discovery since patients may be asymptomatic.
- Detection of subtle lab or imaging abnormalities is crucial in early diagnosis, especially for infiltrative diseases such as AL amyloidosis.
3.3 Guides Clinical Decision-Making
- Clinicians can defer further testing (imaging, biopsy) even with normal bilirubin.
- Facilitates distinguishing acute hepatic failure from early infiltrative or chronic liver disease.
4. Correlation with Other Liver Function Tests (LFTs)
The other LFTs could show early liver involvement even in case of normal bilirubin:
| Test | Early Indicator | Clinical Relevance |
| —————————– | —————- | —————————————- |
| AST / ALT | Mild elevation | Hepatocellular injury |
| ALP | Elevated | Cholestasis or infiltrative disease |
| Albumin | Normal at first | Retained synthetic function |
| Prothrombin time (PT/INR) | Normal | Liver may still be able to make clotting factors
Interpretation: Normal bilirubin with slight elevation of ALP can indicate early infiltrative disease instead of classical hepatitis.
5. Imaging Correlation in Normal Bilirubin
Normal bilirubin does not exclude structural changes in the liver:
- Ultrasound: Can reveal hepatomegaly or nodular surface
- CT/MRI: Can identify early amyloid deposits, infiltrative patterns, or inhomogeneous liver parenchyma
- Elastography: Measures liver stiffness even prior to elevation of bilirubin
Imaging assists in identifying subclinical organ involvement, which is important in systemic illness like AL amyloidosis.
6. Case Example: Preserved Bilirubin in Early AL Amyloidosis
Patient: 61-year-old man with fatigue, mild hepatomegaly
Findings:
- Total bilirubin: Normal
- ALP: Slightly elevated
- Ultrasound: Large liver, irregular surface
- Serum free light chains: High lambda chains
- Liver biopsy: Congo red-positive amyloid deposits
Clinical Relevance: - Normal bilirubin indicated preserved liver function
- Early treatment with chemotherapy averted irreversible damage
- Shows that normal bilirubin does not exclude severe infiltrative disease
7. Differential Diagnosis When Bilirubin is Normal
Despite normal bilirubin, clinicians must think about:
- Infiltrative Disorders
- Amyloidosis, sarcoidosis, lymphoma
- Chronic Cholestatic Diseases in Early Stages
- Primary biliary cholangitis, PSC
- Subclinical Hepatocellular Injury
- Early NAFLD/NASH
- Mild drug-induced liver injury
8. Laboratory Patterns Supporting Early Detection
- Normal bilirubin + elevated ALP: Indicative of cholestasis or infiltration
- Normal bilirubin + mild transaminase elevation: Signals hepatocellular stress
- Normal bilirubin + abnormal serum proteins: Implies systemic disease (amyloidosis)
Clinicians need to consider bilirubin in the context of other labs, imaging, and clinical findings.
9. Implications for Patient Management
- Early Recognition: Identify subclinical disease before bilirubin increases
- Targeted Testing: Emphasize infiltrative, systemic, or metabolic liver disorders
- Monitoring: Follow bilirubin over time to identify disease worsening
- Intervention Planning: Start therapy with preserved synthetic function
10. Role in Prognosis
- Normal bilirubin = improved short-term prognosis, particularly in systemic liver diseases
- In AL amyloidosis, normal bilirubin is associated with reduced risk of hepatic failure
- Permits aggressive therapies such as chemotherapy or stem cell transplantation with decreased risk
11. Emerging Diagnostic Approaches
- Non-invasive imaging: MRI, elastography to identify early infiltration
- Biomarkers: Serum amyloid P component, light chain assays
- Genetic testing: In hereditary infiltrative liver diseases
These methods supplement bilirubin measurement, with an overall understanding of liver function.
12. Clinical Pearls
*
- Normal bilirubin ≠ healthy liver – need to evaluate other LFTs and imaging
- Infiltrative or systemic liver disease early on tends to present without jaundice
- Early identification prevents irreversible damage
- Follow trends over time; even subtle shifts in bilirubin can signal progression of disease
13. Summary Table: Interpretation of Normal Bilirubin in Liver Disease
| Feature | Clinical Significance |
| ——————————- | ——————————————– |
| Normal total bilirubin | Synthetically preserved function, incipient disease |
| Mildly elevated ALP | Potentially infiltrative or cholestatic process |
| Normal transaminases | Hepatocytes relatively preserved |
| Imaging abnormalities | May show subclinical structural abnormalities |
| Early intervention possible | Improved prognosis and organ function preservation |
14. Conclusion
A normal total bilirubin in the context of other liver pathology is of clinical importance:
- Predicts maintained liver synthetic capacity
- Implies early or subclinical illness
- Directs clinicians to explore infiltrative and systemic etiologies, e.g., amyloidosis, sarcoidosis, or lymphoma
- Facilitates early intervention, enhancing outcomes and averting liver injury
Key Takeaways:
- Don’t depend on bilirubin alone to evaluate the liver.
- Consider bilirubin alongside ALP, transaminases, imaging, and systemic findings.
- Normal bilirubin provides a diagnostic window for early detection and treatment.
- Multidisciplinary assessment guarantees correct diagnosis and best management.

