Worsening Jaundice in Hepatic Amyloidosis: A Sign of Cholestatic Liver Failure
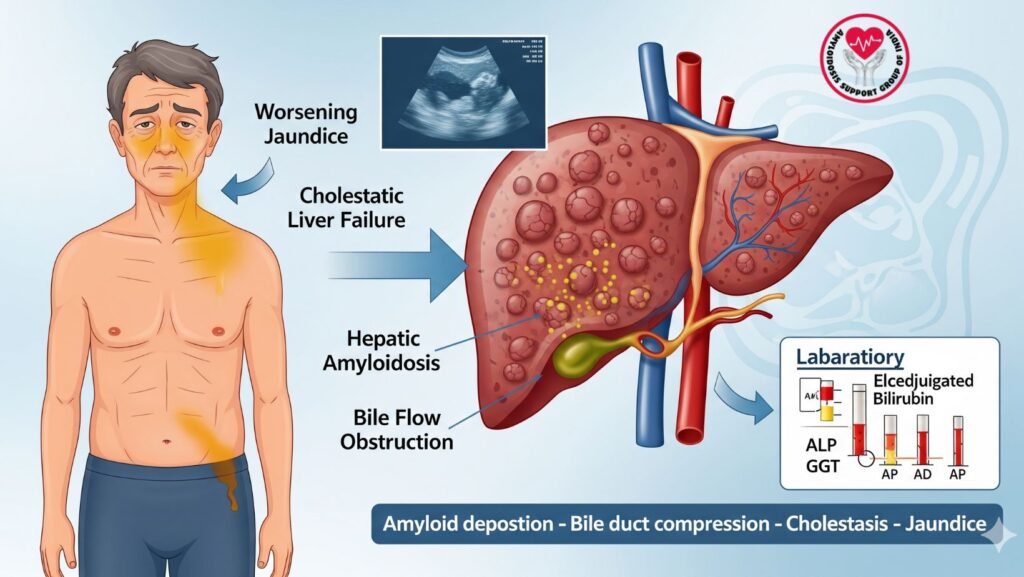
Table of Contents
Introduction
Hepatic amyloidosis is a systemic illness represented by amyloid protein deposition within liver tissue, which interferes with normal architecture and function. Although initial liver involvement may be asymptomatic or mildly abnormal on laboratory tests, progressive jaundice is an ominous sign.
Worsening jaundice is a manifestation of cholestatic liver failure, reflecting severe hepatic involvement. Early identification of this condition is crucial for prognosis, treatment planning, and timely intervention.
This article discusses the pathophysiology of jaundice in hepatic amyloidosis, clinical presentation, laboratory and imaging correlates, and management.
1. Understanding Jaundice in Hepatic Amyloidosis
Jaundice, or yellowing of the eyes and skin, results from increased bilirubin levels. In hepatic amyloidosis, the mechanisms are:
- Amyloid fibril infiltration of hepatocytes – interferes with function of bile canaliculi.
- Compression of bile ducts – obstructs bile flow (cholestasis).
- Hepatocellular dysfunction – decreases bilirubin conjugation and excretion.
Key Point: Progression of jaundice reflects transition from subclinical infiltration to overt cholestatic liver failure.
2. Pathophysiology of Cholestatic Liver Failure in Amyloidosis
Cholestatic liver failure ensues when bile flow is severely impaired, resulting in:
- Buildup of conjugated bilirubin in the blood
- Defective excretion of bile acids, leading to pruritus and malabsorption
- Progressive injury to hepatocytes and synthetic dysfunction
In amyloidosis: - Light-chain deposition in the space of Disse and portal tracts
- Results in compression of sinusoids, decreased hepatic perfusion, and cholestasis
- Severe infiltration can lead to ascites, coagulopathy, and liver failure
3. Clinical Signs of Worsening Jaundice
Patients present with:
- Yellowing of skin and sclera – becomes more intense over time
- Dark urine – secondary to excretion of conjugated bilirubin
- Pale stools – indicating impaired delivery of bile to intestines
- Pruritus – deposition of bile salts in skin
- Fatigue, anorexia, weight loss – systemic effects of liver failure
- Edema or ascites – secondary to hypoalbuminemia and portal hypertension
Clinical Relevance: Progressive worsening jaundice typically portends advanced cholestatic liver failure, necessitating immediate evaluation.
4. Laboratory Findings in Worsening Jaundice
Key laboratory changes include:
| Test | Classic Result in Progressive Hepatic Amyloidosis |
| ———————————— | ———————————————– |
| Total Bilirubin | Raised (primarily conjugated) |
| Direct (Conjugated) Bilirubin | Preponderant increase suggests cholestasis |
| Alkaline Phosphatase (ALP) | Significantly raised due to compression of the bile ducts |
| Gamma-glutamyl transferase (GGT) | Raised, supports cholestatic pattern |
| AST / ALT | Normal or mildly elevated |
| Albumin | Reduced in severe disease |
| Prothrombin Time (PT/INR) | Prolonged due to impaired synthetic function |
Interpretation: The triad of increased conjugated bilirubin, elevated ALP, and mild transaminase increase is characteristic of cholestatic liver damage in amyloidosis.
5. Imaging Findings
Imaging confirms diagnosis and evaluates severity:
- Ultrasound
- Hepatomegaly
- Nodular liver surface
- Mild to moderate ascites
- Unobstructed normal bile ducts (apart from if amyloid does obstruct them)
- CT Scan
- Inhomogeneous liver parenchyma
- Irregular or nodular liver edges
- Portal vein and biliary tree evaluation
- MRI
- Variable T2, T1 hypointense signal
- Diminished parenchymal enhancement
- Identifies early infiltrative patterns
- Nuclear Imaging (Optional)
- SAP scintigraphy to measure systemic amyloid burden
- Assists in directing therapy choices
6. Differential Diagnosis
When jaundice increases in amyloidosis, consider:
- Extrahepatic bile duct obstruction (tumors, gallstones)
- Drug-induced cholestasis
- Viral hepatitis superimposed
- Primary biliary or sclerosing cholangitis
Exclusion of such conditions is important prior to attributing jaundice exclusively to hepatic amyloidosis.
7. Prognostic Significance
Worsening jaundice in hepatic amyloidosis signifies advanced hepatic involvement, corresponding to:
- Higher risk of hepatic failure
- Worse response to chemotherapy or systemic therapy
- Increased chance of complications: ascites, coagulopathy, malnutrition
Key Point: Early detection prior to significant elevation in bilirubin significantly improves the prognosis.
8. Management Strategies
8.1 Supportive Care
- Reversal of electrolyte and fluid imbalances
- Nutritional supplementation, fat-soluble vitamins included
- Pruritus treatment by cholestyramine or antihistamines
8.2 Disease-Directed Therapy
- AL Amyloidosis: Chemotherapy (e.g., bortezomib, cyclophosphamide, dexamethasone)
- Stem Cell Transplantation: Placed in eligible patients to lower amyloid load
- Other systemic treatments as indicated by underlying cause
8.3 Monitoring and Follow-Up
- Serial bilirubin, ALP, liver function tests
- Imaging to track liver size, nodularity, and infiltrative course
- Early identification of complications (ascites, portal hypertension)
9. Case Example: Worsening Jaundice in Hepatic Amyloidosis
Patient: 64-year-old woman with established AL amyloidosis
Course:
- Initially asymptomatic, normal bilirubin
- Evolved over weeks: fatigue, dark urine, jaundice
- Labs: Conjugated total bilirubin 6.5 mg/dL, ALP 450 IU/L
- Imaging: Nodular liver enlargement, mild ascites
- Management: Chemotherapy initiation, supportive treatment of cholestasis
Outcome: - Bilirubin became stable after therapy
- Early detection avoided irreversible hepatic failure
10. Early Recognition: Why It Matters
- Early recognition of worsening jaundice allows for timely intervention
- Distinctly separates cholestatic liver failure from mild hepatic involvement
- Directs treatment urgency and intensity
- Decreases risk of irreversible liver damage and systemic complications
11. Emerging Diagnostic Tools
- MR Elastography: Measures liver stiffness and infiltration
- Quantitative MRI: Identifies early amyloid deposits
- Serum Biomarkers: Free light chains, serum amyloid P component
- Genetic Testing: For hereditary systemic amyloidosis
These tools improve early detection and monitoring, even before jaundice worsens.
12. Clinical Pearls
*
- Deteriorating jaundice in hepatic amyloidosis = advanced cholestatic liver failure
- Screen for conjugated hyperbilirubinemia, increased ALP, and GGT
- Imaging is crucial to determine degree of infiltration
- Intervention early can enhance survival and quality of life
13. Summary Table: Worsening Jaundice in Hepatic Amyloidosis
| Feature | Clinical Significance |
| ———————————————- | ——————————————— |
| Suddenly increasing bilirubin | Means severe cholestatic liver failure |
| Mainly conjugated bilirubin | Establishes cholestasis |
| High ALP/GGT | Indicates bile duct compression/infiltration |
| Imaging: hepatomegaly, nodular liver | Establishes structural liver involvement
| Management: chemotherapy + supportive care | Critical to avoid irreversible liver damage |
14. Conclusion
Worsening jaundice in hepatic amyloidosis is a red flag for progression to cholestatic liver failure. Identification of this clinical sign early:
- Facilitates timely intervention and monitoring
- Directs disease-directed therapy for AL amyloidosis
- Reduces prognosis and avoids irreversible liver damage
Key Takeaways:
- Deteriorating jaundice = advanced hepatic involvement
- Correlation of laboratory and imaging is crucial
- Early diagnosis facilitates supportive care and targeted therapy
- Multidisciplinary management enhances outcomes of systemic amyloidosis

