Multidisciplinary Approach: The Way Forward in the Management of Systemic Amyloidosis Patients
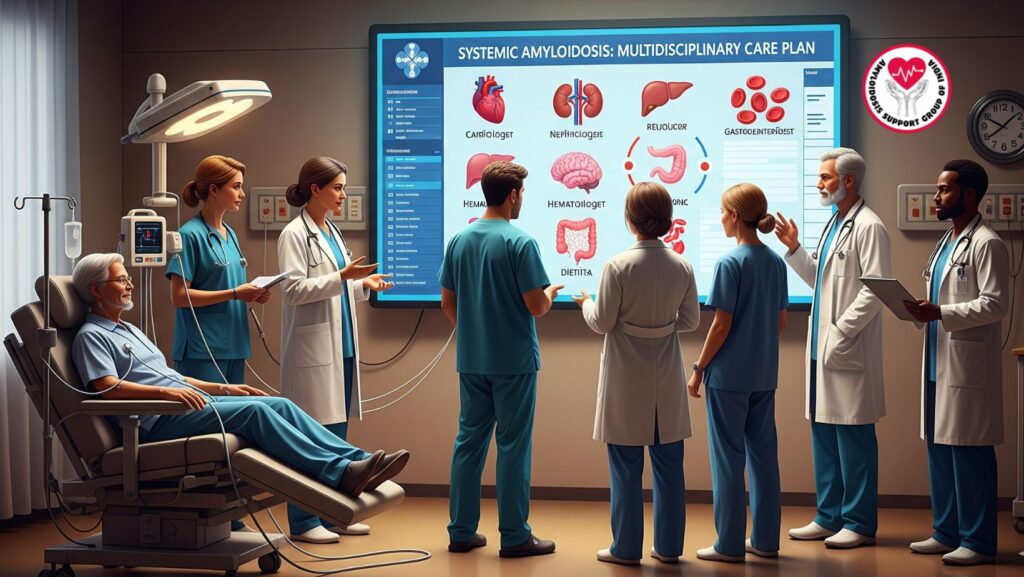
Table of Contents
1. Introduction
Systemic amyloidosis is a multisystem, complex condition resulting from abnormal protein deposition in organs including the heart, kidneys, liver, nervous system, and gastrointestinal system. These deposits cause organ dysfunction which, if left untreated, is inevitably fatal.
Whereas disease-modifying therapy addresses the root cause of protein misfolding—e.g., chemotherapy for AL amyloidosis or transthyretin stabilizers in ATTR amyloidosis—therapy may require a while to have a quantifiable effect. Meanwhile, the patients suffer from substantial symptoms and organ damage, thus demonstrating the importance of comprehensive supportive care.
Multidisciplinary management, provided at centers of excellence, is universally accepted as the gold standard for the treatment of systemic amyloidosis. It guarantees that patients receive organ-specific, coordinated care along with attention to symptom management, rehabilitation, nutrition, and psychosocial issues.
2. Why a Multidisciplinary Approach is Indispensable
Systemic amyloidosis involves several organ systems concurrently. Trying to deal with these diverse manifestations separately can give rise to fragmented care, delayed interventions, and adverse outcomes.
Advantages of a multidisciplinary strategy are:
- Organ-specific coordinated care: Cardiac, renal, hepatic, neurological, and hematologic complications are treated comprehensively.
- Early detection of complications: Specialists track early alterations, avoiding damage to organs beyond reversal.
- Enhanced survival: Stabilizing organ function while type-specific therapy becomes effective improves overall survival.
- Quality of life is improved: Symptom management and rehabilitation enable patients to stay independent.
- Effective use of healthcare: Coordinated care eliminates hospitalizations and unnecessary procedures.
3. Multidisciplinary Team Composition
3.1 Cardiologists
- Screen and treat amyloid-related cardiomyopathy
- Order diuretics, pacemakers, or defibrillators as indicated
- Taper medications with caution to prevent hypotension or arrhythmias
3.2 Nephrologists
- Treat renal complications including proteinuria, nephrotic syndrome, or chronic kidney disease
- Start dialysis or assess for renal transplantation
- Optimize fluid and electrolyte balance
3.3 Neurologists
- Manage peripheral and autonomic neuropathy
- Administer medications for neuropathic pain and autonomic dysfunction
- Monitor CNS involvement and coordinate cognitive rehabilitation
3.4 Hepatologists
- Take care of hepatic amyloidosis, cholestasis, and ascites
- Monitor liver function tests and synthetic function
- Direct nutritional interventions for liver-compromised patients
3.5 Gastroenterologists
- Manage GI symptoms such as diarrhea, constipation, malabsorption, or bleeding
- Administer dietary and medical interventions to preserve nutrition
3.6 Hematologists
- Provide disease-specific therapy in AL amyloidosis
- Manage coagulopathy and anemia or other blood disorders
- Coordinate care with other specialists for safe therapy administration
3.7 Dietitians and Nutritionists
- Develop personalized nutrition plans to treat malnutrition and GI complications
- Provide supplementary vitamins, minerals, and calories as indicated
- Track weight and nutritional status over time
3.8 Palliative Care Specialists
- Alleviate symptoms of pain, fatigue, and GI discomfort
- Provide psychosocial support to patients and families
- Use quality-of-life interventions together with disease-directed therapy
4. Organ-Specific Roles in Multidisciplinary Care
4.1 Cardiac Management
Amyloid deposition makes the heart stiff, resulting in restrictive cardiomyopathy.
Interventions are:
- Diuretics for heart failure
- Monitoring of ECG and cardiac biomarkers
- Device therapy (pacemakers, defibrillators)
- Lifestyle modifications (diet low in salt, activity modification)
4.2 Renal Management
Renal involvement results in proteinuria and chronic kidney disease.
Interventions are:
- ACE inhibitors/ARBs to lower proteinuria
- Diuretics for edema management
- Dialysis for renal impairment
- Nutritional modifications to avoid additional kidney injury
4.3 Neurological Care
Autonomic and peripheral neuropathy result in pain, weakness, orthostatic hypotension, and GI motility.
Interventions include:
- Medications for neuropathic pain (gabapentin, duloxetine)
- Physical therapy and occupational therapy
- Autonomic dysfunction medications (midodrine, fludrocortisone)
4.4 Gastrointestinal Care
GI involvement may result in malabsorption, diarrhea, constipation, and bleeding.
Interventions include:
- Nutritional advising and supplementation
- Prokinetic or antidiarrheal medications
- Parenteral nutrition in severe cases
4.5 Hematology and Coagulopathy Management
Amyloidosis can lead to coagulopathy or anemia.
Interventions include:
- Monitoring clotting profiles
- Blood product transfusions or factor replacement
- Treatment of anemia using erythropoiesis-stimulating agents
5. Benefits of Multidisciplinary Care
- Comprehensive care: All organ systems are monitored and treated together
- Decreased complications: Early treatment avoids organ failure
- Increased survival: Organ support improves tolerance to disease-specific therapy
- Improvement in quality of life: Symptom control enables patients to be independent
- Support from patient and family: Psychological and social support enhances compliance and minimizes stress
6. Centers of Excellence
Multidisciplinary care is best delivered at centers of excellence, which provide:
- Trained specialists in amyloidosis
- Access to advanced diagnostics and clinical trials
- Integrated supportive care services
- Multidisciplinary coordination
- Patient and caregiver education
Patients seen in these centers experience improved outcomes and increased survival compared with those seen in fragmented care.
7. Case Study Example
(Optional section for expansion)
A 62-year-old patient with AL amyloidosis and cardiac, renal, and neuropathic involvement was managed in a multidisciplinary center. With integrated care from cardiology, nephrology, neurology, nutrition, and palliative teams:
- Heart failure stabilized with diuretics
- Kidney function maintained with ACE inhibitors and dialysis support
- Pain and neuropathy controlled with medications and physical therapy
- Nutrition status optimized with dietitian assistance
Outcome: The patient tolerated chemotherapy well, had partial remission, and preserved quality of life.
8. Future Directions in Multidisciplinary Care
- Digital health: Distant monitoring of cardiac, renal, and neurological function
- Telemedicine: Availability of multidisciplinary consultation for patients in rural communities
- Wearable devices: Ongoing monitoring of vital signs and arrhythmias
- Personalized medicine: Individualizing supportive interventions based on patient-specific organ involvement
9. Conclusion
A multidisciplinary approach is the core in systemic amyloidosis treatment. By combining supportive care, organ-specific treatment, and disease-directed therapy at centers of excellence, patients achieve:
- Stabilized organ function
- Enhanced survival
- Improved quality of life
- Decreased hospitalizations
For healthcare providers, a team-based, coordinated care model is the best approach to address the multisystemic, complex challenges of systemic amyloidosis.
Key Takeaways:
- Multidisciplinary care is crucial for best results
- Excellence centers offer concordant and targeted interventions
- Interdisciplinary collaboration between cardiology, nephrology, neurology, hematology, gastroenterology, and palliative care assures whole-patient management
- Synthesis of supportive care with disease-related therapy optimizes survival and quality of life

