Beta-Blockers in Cardiac Amyloidosis: Benefits, Risks, and Clinical Considerations
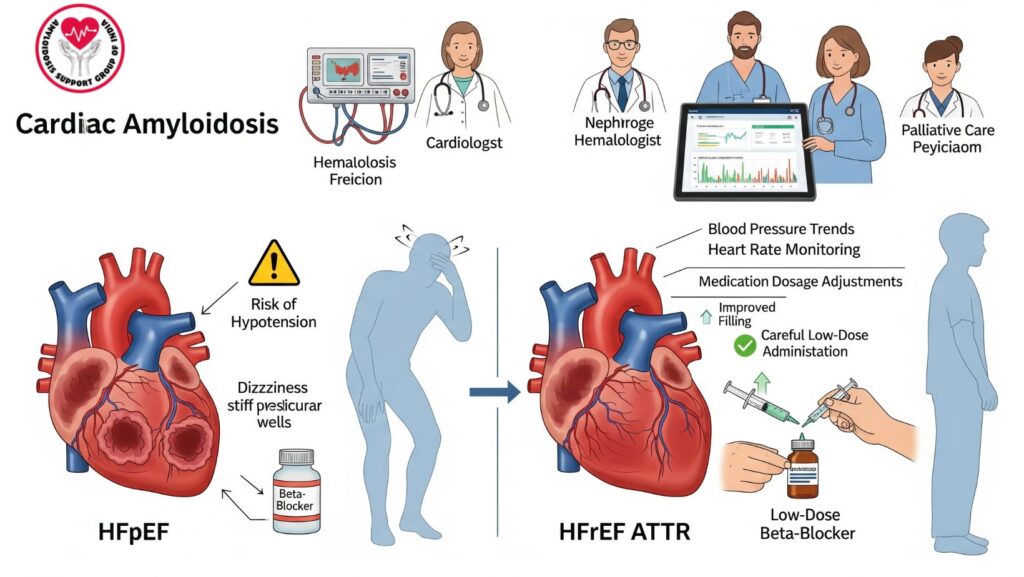
Table of Contents
1. Introduction
Cardiac amyloidosis (CA) is an infiltrative cardiomyopathy due to amyloid deposits in the myocardium, resulting in stiff ventricles, diastolic dysfunction, arrhythmias, and heart failure.
Beta-blockers, which are routine therapy for heart failure overall populations, have limited and subtle roles in CA. Although they decrease heart rate and might improve survival in certain patients, they decrease cardiac output and cause symptomatic hypotension, particularly in restrictive physiology.
The role, risks, benefits, and clinical considerations of beta-blockers in CA are discussed in this article, with emphasis on HFpEF vs HFrEF, ATTR vs AL amyloidosis, and multidisciplinary management.
2. Pathophysiology of Cardiac Amyloidosis Pertinent to Beta-Blocker Use
Amyloid deposition leads to:
- Decreased ventricular compliance → diastolic dysfunction
- Decreased stroke volume → cardiac output is rate-dependent
- Conduction defects → AV block or bradyarrhythmias
- Autonomic impairment → disrupted blood pressure regulation
Beta-blocker implications: - Negative chronotropic effects can decrease cardiac output
- Can exacerbate fatigue, dizziness, hypotension, or syncope
- Low-dose beta-blockers can be tolerated in certain HFrEF patients (EF <40%)
3. Beta-Blockers in HFpEF versus HFrEF in CA
3.1 HFpEF (Preserved EF)
- Frequent in CA
- Diastolic dysfunction prevails; EF is preserved
- Reduction of heart rate can reduce cardiac output and lead to symptomatic hypotension
- Routine use of beta-blockers is usually not indicated, unless for rate control in AF
3.2 HFrEF (Reduced EF)
- In severe CA
- Low-dose beta-blockers can enhance survival and ventricular filling in certain ATTR patients
- Needs careful titration and monitoring for bradycardia and hypotensionomet
4. Clinical Indications and Patient Selection
Potential indications:
- Control of atrial fibrillation or flutter rate
- Relief of symptomatic palpitations
- Low-dose treatment in HFrEF ATTR patients with EF <40%
Contraindications / Cautions: - Advanced HFpEF with reduced stroke volume
- Symptomatic hypotension or syncope
- Severe conduction disease (high-grade AV block)
- Renal insufficiency leading to hypotension
5. Risks and Adverse Effects
5.1 Symptomatic Hypotension
- Decreased heart rate → decreased cardiac output
- May worsen fatigue, dizziness, syncope
5.2 Bradyarrhythmias
- AV block or sinus node dysfunction patients are high-risk
- Pacemaker prior to initiation may be needed
5.3 Exercise Intolerance
- Decreased heart rate response can restrict activity tolerance in CA patients
6. Beta-Blocker Selection and Titration
- Begin very low doses
- Titrate slowly with close monitoring of BP, heart rate, and renal function
- Agents of choice can be bisoprolol or carvedilol, titrated carefully
- Do not stop abruptly → risk of rebound tachycardia or arrhythmia
7. Alternative Approaches in Patients Unable to Tolerate Beta-Blockers
- Amiodarone for rate control in AF
- Pacemaker implantation for bradyarrhythmias
- Non-pharmacologic therapy: hydration management, compression stockings
- Disease-specific treatment to decrease amyloid burden:
- AL amyloidosis → chemotherapy, proteasome inhibitors, stem cell transplantation
- ATTR amyloidosis → tafamidis, diflunisal, RNA silencing
8. Multidisciplinary Management
Best care entails:
- Cardiologists → follow-up EF, beta-blocker titration, HF symptom management
- Hematologists → treatment of AL amyloidosis
- Electrophysiologists → management of pacemaker / ICD
- Nephrologists → renal function, fluid status
- Palliative care and nutritionists → quality of life, dietary optimization
Benefits: minimizes adverse events, enhances tolerability, and maximizes outcomes
9. Monitoring and Safety Considerations
- BP and heart rate daily or at every visit
- ECG if bradyarrhythmias or AV block
- Renal function and electrolytes often
- Check for symptoms of hypotension, fatigue, and exercise intolerance
- Biomarkers (BNP, troponin) can monitor cardiac stress
10. Patient Education
- Identify early hypotension and bradycardia signs
- Stand up slowly to avoid dizziness or falls
- Report syncope, severe fatigue, or palpitations urgently
- Follow fluid, salt, and exercise advice
- Know purpose of beta-blockers and titration schedule
11. Emerging Therapies and Research
- Tafamidis, patisiran, inotersen enhance ATTR outcomes and potentially enable improved beta-blocker tolerance
- Investigation of new agents that decrease myocardial amyloid load
- Digital monitoring of blood pressure and heart rate for safer titration
12. Prognosis and Outcomes
- Beta-blockers in CA have limited application, mostly in selected HFrEF ATTR patients or for rate control
- Symptomatic hypotension is a frequent limiting factor
- Early disease-specific therapy enhances cardiac function and potential beta-blocker tolerance
- Multidisciplinary care enhances functional status, survival, and quality of life
13. Case Example (Optional)
A 66-year-old patient with ATTR amyloidosis and HFrEF (EF 35%):
- Started on low-dose carvedilol
- BP checked daily; mild fatigue noted
- Dose titrated slowly over 6 weeks
- Outcome: Enhanced ventricular filling, decreased palpitations, no symptomatic hypotension
- Multidisciplinary team consisted of cardiology, nephrology, and nutrition
14. Conclusion
Beta-blockers play a niche but critical role in cardiac amyloidosis:
Key Takeaways:
- Overall not tolerated in HFpEF, potentially causes hypotension
- Low-dose treatment may help HFrEF ATTR patients
- Titration, monitoring, and multidisciplinary care must be careful and attentive
- Disease-specific treatment can maximize beta-blocker safety and efficacy

