Volume Overload in Cardiac Amyloidosis: The Role of Loop Diuretics

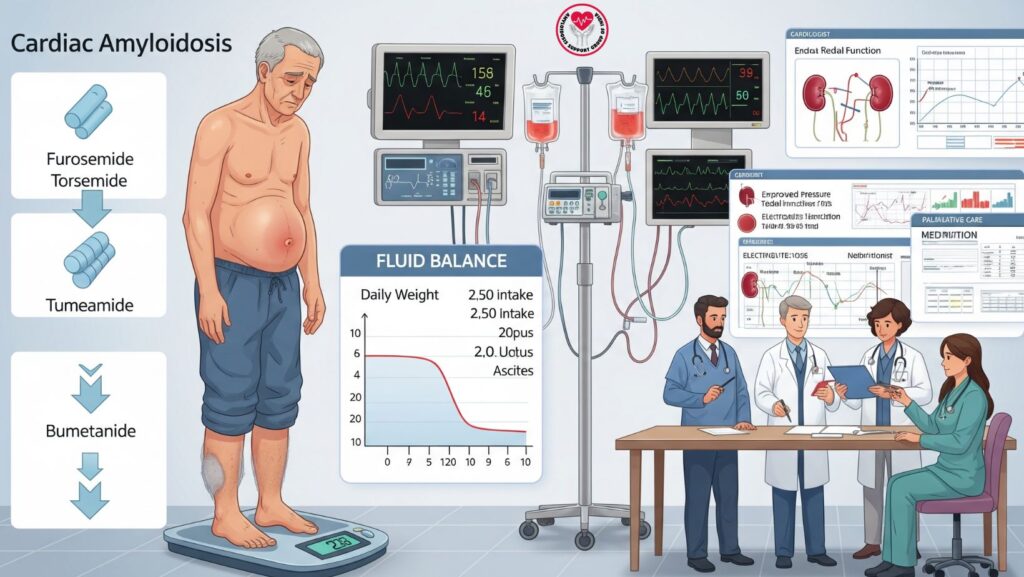
Table of Contents
1. Introduction
Cardiac amyloidosis (CA) is a group of infiltrative cardiomyopathies defined by amyloid deposition within the myocardium, resulting in stiff ventricles, diastolic dysfunction, and restrictive heart failure. Among the most frequent clinical issues in CA is volume overload, expressed as peripheral edema, ascites, and pulmonary congestion.
Loop diuretics, such as furosemide, torsemide, and bumetanide, are the first-line treatment to control volume overload. They relieve congestion, alleviate symptoms, and ensure quality of life. This article discusses loop diuretic therapy strategies, dosing, combination therapy, monitoring, and supportive care in CA.
2. Pathophysiology of Volume Overload in CA
Amyloid deposition within the heart results in:
- Stiff ventricles → diastolic dysfunction → high filling pressures
- Low stroke volume → compensatory fluid retention
- Renal congestion → impaired natriuresis
- Neurohormonal activation → RAAS and sympathetic activation
Clinical manifestations: - Peripheral edema (legs, ankles, sacral region)
- Ascites
- Pulmonary congestion
- Weight gain
- Dyspnea and exercise intolerance
Loop diuretics act on the kidney’s thick ascending loop of Henle, inducing natriuresis and diuresis, which reduces intravascular and interstitial fluid.
3. Loop Diuretics in Cardiac Amyloidosis
3.1 Furosemide
- Most commonly used loop diuretic
- Sudden onset (oral: 30–60 min, IV: 5 min)
- Action: 4–6 hours by mouth
- Effective for acute decompensation or chronic control
3.2 Torsemide
- Longer half-life (oral: ~3–4 hours, with activity up to 12 hours)
- More consistent absorption than furosemide
- Frequently used in chronic outpatient care
3.3 Bumetanide
- Very potent (1 mg ≈ 40 mg furosemide)
- Effective in resistant edema or late-stage CA
- Available in oral and IV forms
4. Dosing and Titration Strategies
- Begin with the minimum effective dose
- Oral furosemide: 20–40 mg once per day, titrate with response
- Torsemide: 10–20 mg once per day
- Bumetanide: 0.5–1 mg once or twice per day
- Titrate slowly to balance fluid loss with risk of hypotension and renal impairment
- IV bolus or continuous infusion in acute decompensated CA
Key principle: CA patients are preload-dependent, therefore aggressive diuresis can aggravate hypotension and renal perfusion.
5. Combination Therapy
- Combined with SGLT2 inhibitors → synergistic natriuresis and fluid management
- Low-dose GDMT (ACEIs, ARBs, ARNIs, beta-blockers) → if tolerated, for long-term cardiac protection
- Mineralocorticoid receptor antagonists → add cautiously for resistant edema
- Disease-specific therapy → AL (chemotherapy, stem cell transplant), ATTR (tafamidis, RNA therapy) decreases cardiac amyloid burden
6. Monitoring and Safety Considerations
Monitor:
- Blood pressure → avoid symptomatic hypotension
- Renal function (creatinine, eGFR)
- Electrolytes → potassium, sodium, magnesium
- Weight and fluid balance → daily at home or clinic
- Signs of dehydration → dry mucosa, dizziness, hypotension
Adverse effects: - Hypotension
- Electrolyte imbalance → hypokalemia, hyponatremia
- Renal impairment
- Ototoxicity (rare, high IV doses)
7. Supportive Care Measures
- Low-salt diet → maximize diuretic effect
- Compression stockings → minimize peripheral edema
- Gradual mobilization → avoid orthostatic hypotension
- Patient education → identify fluid overload and dehydration
- Regular follow-up → titrate diuretic doses according to weight and symptoms
8. Multidisciplinary Approach
Volume overload in CA is optimized by having a team approach:
- Cardiologists → maximize heart failure treatment, titrate diuretics
- Nephrologists → manage renal function, avoid acute kidney injury
- Hematologists → management of AL amyloidosis
- Nutritionists → regulate salt and fluid intake
- Palliative care → symptom control, quality of life
Advantages: enhanced outcomes, fewer hospitalizations, improved tolerance to drugs.
9. Emerging Strategies for Refractory Edema
*
- Sequential nephron blockade: loop + thiazide diuretics combination
- Ultrafiltration → for diuretic-resistant fluid overload
- SGLT2 inhibitors → adjunctive therapy for chronic volume management
- Optimizing disease-specific therapy → decreases chronic fluid retention
10. Prognosis and Outcomes
*
- Proper volume management enhances symptoms, exercise tolerance, and quality of life
- Indiscriminate diuresis in the absence of monitoring may exacerbate hypotension and renal impairment
- Multidisciplinary supportive treatment enhances long-term safety and outcomes
- Early intervention decreases hospitalizations due to decompensated heart failure
11. Case Example (Optional)
70-year-old patient with ATTR cardiac amyloidosis:
- Had ankle edema, ascites, and mild dyspnea
- Initiated on oral furosemide 20 mg daily, which was titrated to 40 mg
- BP, weight, and renal function monitored weekly
- Combined with SGLT2 inhibitor and low-salt diet
- Outcome: Marked reduction of edema, BP control, enhanced exercise tolerance
12. Conclusion
Loop diuretics continue to be the cornerstone for controlling volume overload in cardiac amyloidosis:
Key Takeaways:
- Furosemide, torsemide, and bumetanide are effective symptom relievers
- Careful titration and observation are required
- Combination with SGLT2 inhibitors and disease-specific therapy enhances outcomes
- Multidisciplinary supportive care promotes safety, efficacy, and quality of life

