Dietary Management in Cardiac Amyloidosis: Sodium and Fluid Limitations in Heart Failure
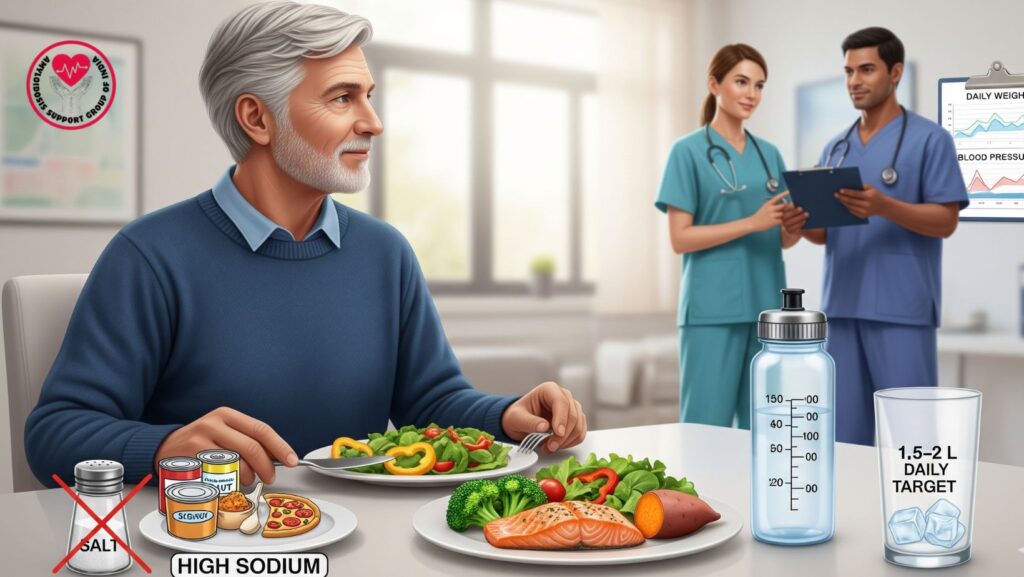
Table of Contents
1. Introduction
CA is a restrictive cardiomyopathy defined by amyloid deposition within the myocardium with consequences of stiff ventricles, diastolic dysfunction, and heart failure.
Heart failure in CA tends to be present with volume overload, such as edema, ascites, and pulmonary congestion. Although pharmacologic therapy (loop diuretics, SGLT2 inhibitors) is foundational, dietary management is an important ancillary approach.
This review is on fluid and sodium limitation, pragmatic strategies, patient teaching, and incorporation with total supportive care in CA.
2. Pathophysiology of Fluid Accumulation in CA
- Stiff ventricles and diastolic dysfunction → increased filling pressures
- Neurohormonal activation → RAAS and sympathetic system enhance fluid accumulation
- Low cardiac output → sodium and water retention by kidneys
- Clinical manifestations:
- Peripheral edema
- Ascites
- Pulmonary congestion
- Weight gain
Dietary changes address volume management, decreasing congestion and enhancing exercise tolerance and quality of life.
3. Sodium Restriction in Cardiac Amyloidosis
3.1 Recommended Intake
- Restrict sodium to <2 g/day (~5 g salt)
- Steer clear of high-sodium packaged foods: canned soups, sauces, frozen foods, chips, and fast food
3.2 Benefits
- Decreases intravascular and interstitial fluid accumulation
- Increases loop diuretic effectiveness
- Prevents excessive weight gain and edema
3.3 Practical Tips
- Read nutrition labels for sodium content
- Use herbs, spices, and lemon juice in place of salt
- Opt for fresh fruits, vegetables, lean proteins
- Restrict restaurant and takeout meals
4. Fluid Restriction in Cardiac Amyloidosis
4.1 Recommended Intake
- Restrict fluid intake to 1.5–2 L/day
- Includes all drinks, soups, and water content in foods
4.2 Benefits
- Prevents pulmonary congestion and peripheral edema
- Reduces hospitalizations for decompensated heart failure
- Improves symptom management in late-stage CA
4.3 Practical Tips
- Monitor fluid intake through a daily log
- Take fluids in between meals rather than large amounts at one time
- Use ice chips or sugar-free gum to manage thirst
- Restrict high-water-content fruits when needed
5. Integration with Pharmacologic Therapy
- Loop diuretics: synergize with sodium and fluid restriction
- SGLT2 inhibitors: augment natriuresis and volume control
- Low-dose GDMT: can be better tolerated with proper dietary management
- Monitoring: daily weight, blood pressure, renal function, and electrolytes
6. Nutritional Considerations
- Protein intake: sufficient protein maintains muscle mass and overall well-being
- Potassium: monitor if on diuretics; modify intake via fruits and vegetables
- Calcium and magnesium: maintain dietary intake to avoid electrolyte imbalance
- Balanced diet: emphasize fresh produce, whole grains, lean meats, and healthy fats
7. Multidisciplinary Approach
- Cardiologists: titrate diuretics and monitor fluid status
- Dietitians/Nutritionists: customize sodium and fluid restriction regimens
- Nurses: reinforce patient education and daily assessment
- Palliative care: facilitate adherence, comfort, and symptom control
- Family/caregivers: assist implementation of dietary strategies at home
8. Patient Education and Adherence
- Teach on reading food labels and portion control
- Describe the importance of fluid restriction for symptom relief
- Promote daily weight monitoring and reporting notable changes
- Talk about strategies for coping with thirst and hunger
- Enforce compliance through follow-up and support groups
9. Monitoring and Safety
*
- Weight monitoring: daily to identify fluid retention
- BP and heart rate: prevent hypotension or dehydration
- Renal function: modify fluid and sodium intake if kidney function impairs
- Electrolytes: especially potassium and sodium
- Symptoms: fatigue, dizziness, edema
10. Emerging Dietary Strategies
- Personalized sodium goals according to clinical status
- Adjustment of fluid intake in advanced heart failure or hyponatremia
- Patient-tailored meal planning for compliance
- Application of digital apps for monitoring of fluid and sodium intake
11. Prognosis and Outcomes
- Correct diet management lowers symptoms, enhances functional capacity, and lessens hospitalizations
- Acts synergistically with medications and disease-related treatments
- Facilitates long-term quality of life and patient independence
12. Case Example (Optional)
A 68-year-old patient with ATTR cardiac amyloidosis:
- NYHA class II symptoms, peripheral edema, and mild ascites
- Utilized sodium restriction <2 g/day and fluid restriction 1.5 L/day
- Combined with low-dose furosemide and SGLT2 inhibitor
- Outcome: Decreased edema, better exercise tolerance, stable BP, fewer hospitalizations
13. Conclusion
Dietary management is essential supportive care in cardiac amyloidosis:
Key Takeaways:
- Sodium restriction (<2 g/day) and modest fluid restriction (<1.5–2 L/day) are recommended
- Increases efficacy of diuretics and other heart failure treatments
- Calls for education of patients, monitoring, and multidisciplinary care
- Enhances symptom management, quality of life, and hospitalization

