Implantable Cardioverter-Defibrillators (ICDs) in Cardiac Amyloidosis: Do They Really Help?
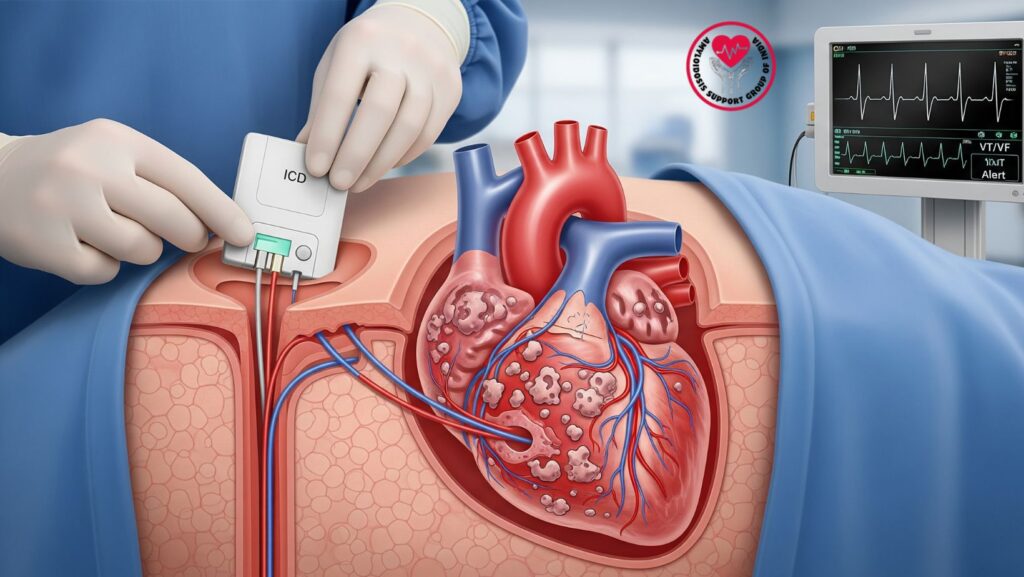
Table of Contents
1. Introduction
Cardiac amyloidosis (CA) is an infiltrative cardiomyopathy due to the deposition of amyloid fibrils in the myocardium, resulting in diastolic dysfunction, restrictive physiology, arrhythmias, and heart failure.
Of all the clinical problems, sudden cardiac death (SCD) is one of the most dreaded complications. This brings us to an important question:
Do implantable cardioverter-defibrillators (ICDs) enhance survival in CA, or do they have minimal value in this heterogeneous disease?
This article discusses the evidence, controversies, patient selection, and clinical considerations for the use of ICD in CA.
2. Mechanisms of Arrhythmias and Sudden Death in CA
- Amyloid infiltration of conduction system → AV block, sinus node dysfunction
- Scar-like substrate → propensity to ventricular tachyarrhythmias
- Electromechanical dissociation (EMD) / pulseless electrical activity (PEA) → frequent etiology of SCD in CA
- Progression of heart failure → increases risk of bradyarrhythmias and refractory hypotension
In contrast to other cardiomyopathies, SCD in CA is frequently caused by EMD/PEA, something that ICDs are powerless to prevent. That is at the heart of the argument regarding ICD usefulness in this condition.
3. ICDs in historical perspective: Heart Failure vs CA
- In ischemic cardiomyopathy or dilated cardiomyopathy non-ischemic, ICDs have been shown to save lives by avoiding ventricular tachyarrhythmias.
- In cardiac amyloidosis, however:
- Arrhythmias are not necessarily the predominant cause of death
- SCD can occur due to electromechanical dysfunction instead of shockable rhythms
- Outcomes of device therapy are less well defined Amyloidosis
4. Current Guidelines and Recommendations
–
- ACC/AHA/HRS guidelines: ICDs may be considered for amyloidosis patients who otherwise fulfill traditional ICD indications.
- ESC guidelines: No clear statement because of absence of randomized data.
- Expert consensus:
- ICDs should not be implanted universally in CA patients
- Might be beneficial in well-chosen patients with high arrhythmia risk
5. Evidence from Clinical Studies
5.1 Observational Data
- A number of small retrospective reports have demonstrated:
- ICDs reliably terminated ventricular tachycardia (VT) in some CA patients
- Nevertheless, no consistent survival benefit was established
- Proportionally, many died from progressive heart failure or EMD
5.2 ATTR vs AL Amyloidosis
- Wild-type ATTR patients with intact EF are more likely to die from VT/VF
- AL patients usually die from multi-organ dysfunction, hence the ICDs become less effective
5.3 Key Findings
- Arrhythmic death might be prevented by ICDs in selected ATTR patients
- They do not avert deaths due to EMD or refractory heart failure
- Benefit is most probable when:
- EF <35% with ventricular arrhythmias
- History of sustained VT or resuscitated cardiac arrest
6. Indications for Considering ICD in CA
6.1 Secondary Prevention
- Strongest evidence for ICD implantation in CA
- Indicated if patient has:
- Survived sudden cardiac arrest due to VT/VF
- Sustained VT with hemodynamic compromise
6.2 Primary Prevention
- More controversial
- Consider in:
- ATTR patients with high arrhythmia burden
- EF <35% despite optimal therapy
- Documented nonsustained VT on Holter monitoring
6.3 Conditions Where ICD is Not Indicated
- Advanced heart failure (NYHA IV) with short life expectancy (<1 year)
- AL amyloidosis with multi-organ involvement
- Recurrent EMD/PEA instead of VT/VF patients
7. Risks and Pitfalls of ICDs in CA
- Procedural risks: increased due to frailty, risk of bleeding, coagulopathy
- Lead-related complications: challenging lead implantation in infiltrated myocardium
- Inappropriate shocks: secondary to atrial arrhythmias (AF is frequent in CA)
- Limited survival benefit: high competing risk of non-arrhythmic mortality
8. Alternative and Adjunctive Therapies
- Amiodarone: frequently utilized for ventricular and atrial arrhythmias
- Beta-blockers: poor tolerance in CA because of hypotension
- Anticoagulation: imperative in AF, irrespective of CHA₂DS₂-VASc score
- Supportive care: fluid and sodium restriction, volume control with diuretics
- Disease-modifying therapy: tafamidis (ATTR), chemotherapy (AL), gene-silencing drugs
9. Multidisciplinary Care Model
- Decisions for ICD in CA need to include:
- Cardiology (electrophysiology): assessment of arrhythmia risk
- Amyloidosis specialists: estimation of disease stage and prognosis
- Palliative care: quality of life and goals of care
- Nephrology/Hematology: comorbidity management
10. Case Examples
Case 1 – ATTRwt Patient:
- 70-year-old male, ATTRwt, EF 40%, frequent nonsustained VT
- ICD implanted for primary prevention
- Outcome: appropriate ICD shocks at 6 months, survival benefit
Case 2 – AL Patient: - Female, 62 years old, AL amyloidosis with multi-organ involvement, EF 25%
- ICD implanted following syncope
- Outcome: no shocks administered, died of multi-organ failure at 9 months
11. Patient Education and Shared Decision-Making
Patients need to be informed about:
- Uncertainty of ICD benefit in CA
- Risk of inappropriate shocks
- Need for regular monitoring and follow-up
- Significance of continuous disease-specific treatment
- Quality of life issues
12. Future Directions
- Requirement of prospective trials on ICDs in CA
- Usage of wearable defibrillators as a bridge in new onset patients
- Investigation of biomarkers and imaging predictors of risk of arrhythmia
- Blending with emerging amyloidosis treatments may change outcomes
13. Conclusion
- ICDs have a limited but significant role in cardiac amyloidosis
- Optimal for secondary prevention in subjects with previous VT/VF
- Could be an option for selected patients with ATTR at high arrhythmia risk
- Provide unknown survival benefit in advanced disease because of competing hazards
- Need careful multidisciplinary assessment and shared decision-making
Key Takeaway:
ICDs are not universally favorable in CA, but they are still an option for appropriately chosen patients, especially for secondary prevention in ATTR-related disease.

