“SGLT2 Inhibitors in Renal Amyloidosis: Benefits for Kidney and Heart Involvement”
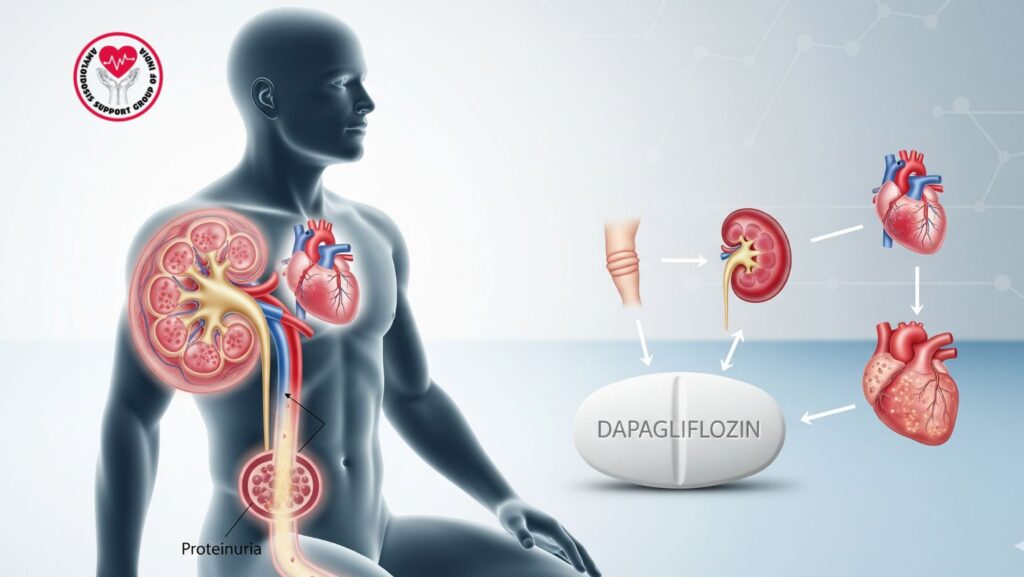
Table of Contents
1. Introduction
Renal amyloidosis, frequently secondary to AL or AA amyloid deposition, usually results in proteinuria, edema, and worsening kidney function. Cardiac involvement is frequent, particularly in AL and ATTR amyloidosis, thereby inducing a cardiorenal syndrome situation.
SGLT2 inhibitors, initially used to manage diabetes, have become renoprotective and cardioprotective agents and are highly appealing in amyloidosis patients with concomitant heart and kidney involvement.
This review discusses the mechanisms, advantages, dosage, monitoring, and clinical evidence of SGLT2 inhibitors in renal amyloidosis.
2. Renal Amyloidosis
2.1 Pathophysiology
Amyloid fibrils accumulate in the kidneys, with a predilection for:
- Glomeruli → causing proteinuria
- Interstitium and vessels → progressive CKD
These deposits interfere with regular renal filtration, leading to: - Severe proteinuria
- Hypoalbuminemia and edema
- Slow loss of glomerular filtration rate
2.2 Clinical Presentation
The patients can present with:
- Peripheral edema (ankles, periorbital)
- Ascites in more severe cases
- Fatigue and decreased exercise tolerance
- Laboratory results: proteinuria >3.5 g/day, low serum albumin
Case Example:
A 62-year-old man with AL amyloidosis had nephrotic-range proteinuria and minimal cardiac involvement. Use of an SGLT2 inhibitor was added to improve markers of kidney function and decrease edema within 3 months.
3. Mechanism of Action of SGLT2 Inhibitors
- Renal glucose reabsorption blockade: Decreases hyperfiltration and proteinuria
- Natruiretic effect: Facilitates sodium excretion, decreasing fluid overload
- Cardiorenal protection: Ameliorates heart and kidney outcomes in patients with CKD and heart failure
- Metabolic benefits: Mild lowering of blood pressure and weight
In amyloidosis, these benefits are particularly useful for patients with renal and cardiac involvement, benefiting proteinuria, edema, and cardiorenal stress at the same time.
4. Indications and Benefits in Renal Amyloidosis
4.1 Indications
- Patients with AL or ATTR amyloidosis and CKD
- Proteinuria despite conventional treatment (RAS blockers, diuretics)
- Concomitant heart involvement (heart failure with preserved or reduced ejection fraction)
4.2 Benefits
- Albuminuria reduction
- Slower CKD progression
- Reduced risk of hospitalization for heart failure
- Enhanced quality of life through reduction of edema
Clinical Tip:
SGLT2 inhibitors may be added to RAS blockers and diuretics safely with vigilant monitoring of kidney function and volume status.
5. Dosing and Administration
*
Common SGLT2 inhibitors: dapagliflozin, empagliflozin, canagliflozin
- Standard dose:
- Dapagliflozin: 10 mg daily
- Empagliflozin: 10 mg daily
- Canagliflozin: 100 mg once a day
- Take in morning with or without food
- Adjust therapy according to kidney function (eGFR) and fluid status
5.1 Combination Therapy
- May be combined with RAS blockers, loop diuretics, and disease-specific amyloidosis therapy
- Monitor for hypotension or volume depletion in patients with cardiac involvement
6. Monitoring During Therapy
- Kidney function: Creatinine, eGFR, albuminuria
- Electrolytes: Sodium, potassium, magnesium
- Volume status: Watch for hypotension, dizziness, dehydration
- Heart function: Signs of heart failure or fluid overload
Tip: Begin at low-normal kidney function; use cautiously in advanced CKD without nephrology consultation.
7. Safety and Adverse Effects
- Volume depletion/hypotension – particularly with diuretics
- Genital mycotic infections – more likely to occur in diabetics
- Ketoacidosis – unusual, in patients primarily with diabetes
- Electrolyte imbalances – follow potassium and sodium levels
Case Example:
A 60-year-old woman with ATTR amyloidosis initiated empagliflozin; mild hypotension developed but was corrected with fluid management and monitoring of the dose.
8. Integration with Disease-Specific Therapy
- In AL amyloidosis: Pair SGLT2 inhibitors with chemotherapy or stem cell transplantation
- In ATTR amyloidosis: Pair with tafamidis or patisiran therapy
- Aim: symptomatic improvement, proteinuria reduction, and cardiorenal protection
9. Case Studies and Real-World Outcomes
- Case 1: 65-year-old man with renal and cardiac AL amyloidosis; dapagliflozin decreased proteinuria by 25% at 3 months and alleviated peripheral edema
- Case 2: 58-year-old woman with ATTR amyloidosis; empagliflozin maintained kidney function and decreased heart failure hospitalizations
Observation: Timely use of SGLT2 inhibitors in cardiorenal amyloidosis enhances renal outcome, heart function, and quality of life.
10. Supportive Measures
- Use sodium restriction (<2 g/day)
- Monitor fluid intake
- Proceed with diuretics with caution for edema
- Patient education regarding hydration, prevention of infection, and weight monitoring
11. Future Directions
- Studies on novel SGLT2 inhibitors with greater renal and cardiac effects
- Tailor therapy to amyloid type, kidney disease, and heart function
- Add-on to emerging anti-amyloid treatments might further enhance outcome
12. Conclusion
SGLT2 inhibitors offer a twofold benefit in renal amyloidosis patients with simultaneous cardiac involvement, lowering albuminuria, retarding CKD progression, and enhancing heart performance.
By ensuring selective patient selection, monitoring, and combination with other treatments, SGLT2 inhibitors are a useful asset in the treatment of cardiorenal complications in amyloidosis.

