Non-Pharmacological Treatments for Orthostatic Hypotension in Amyloidosis
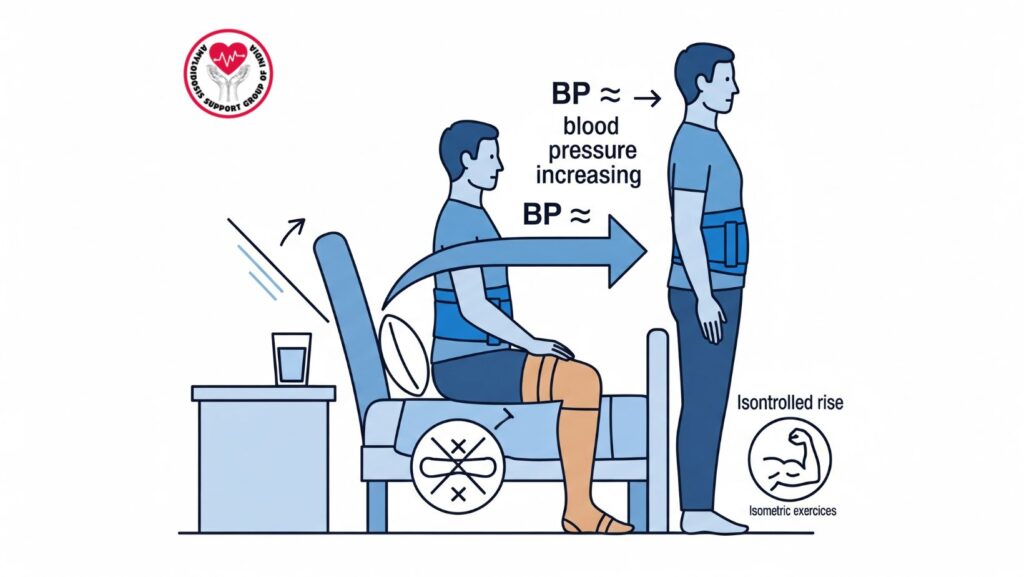
Table of Contents
Introduction
Orthostatic hypotension (OH) is a frequent complication in systemic amyloidosis, especially if autonomic nervous system function is compromised. OH is diagnosed by a decrease in systolic blood pressure ≥20 mmHg or diastolic blood pressure ≥10 mmHg within 3 minutes of standing. Symptoms of dizziness, lightheadedness, blurred vision, and syncope can impact significantly on quality of life and place patients at risk for falls.
Although pharmacologic therapy with drugs such as midodrine or fludrocortisone may be helpful, non-pharmacological interventions are the mainstay of management, especially in mild-to-moderate OH, or as an adjunct to medications.
This article discusses practical non-drug approaches to the management of OH in amyloidosis and offers information for patients, caregivers, and clinicians.
1. Review of Medication
Some drugs can exacerbate orthostatic hypotension by reducing blood pressure or disrupting autonomic function. Regular review is critical:
- Diuretics can contribute to volume depletion.
- Antihypertensives like alpha-blockers, beta-blockers, or ACE inhibitors can also cause OH.
- Chemotherapy or supportive drugs can also affect blood pressure.
Recommendations
- Weigh all medications with the physician.
- Non-essential drugs causing hypotension should be adjusted or stopped.
- Medications may be taken at alternate times to minimize postural symptoms.
2. Adjustments of Fluid and Salt Intake
Physiological intravascular volume is important to prevent OH.
- Encourage adequate intake of water, usually 2–3 liters/day, unless limited for cardiac or renal conditions.
- Frequent small sips are often better than a large amount all at once.
Salt Intake
- Dietary sodium intake can be increased to help increase plasma volume.
- Heart failure and renal patients should make salt adjustments under medical guidance.
3. Slow Position Changes
Quick transitions from recumbent or sitting to upright positions can lead to OH attacks.
Techniques
- Sit on the edge of bed for 1–2 minutes before standing.
- Arise gradually, using leg muscles to aid venous return.
- Steer clear of sudden bending or twisting when standing.
4. Physical Maneuvers
Simple maneuvers may enhance venous return and alleviate symptoms:
- Crossing legs: Crossing legs while standing elevates vascular resistance.
- Squatting or brief bending forward: Aids in preservation of blood pressure until stable.
- Isometric exercises: Muscle tension in calf and thigh when standing.
5. Head-of-Bed Elevation
- Raising the head of the bed 10–20 degrees decreases nocturnal fluid shifts.
- Can help alleviate morning orthostatic symptoms.
- Can be added to morning mobilization in a gradual fashion.
6. Compression Garments
Compression garments enhance venous return and decrease lower extremity pooling:
- Knee-high or thigh-high stockings: Exert 20–30 mmHg pressure.
- Abdominal binders: Decrease splanchnic pooling, especially beneficial in autonomic dysfunction.
- Proper sizing is important to prevent constriction or discomfort.
7. Graded Exercise
Physical exercise enhances vascular tone and cardiovascular reflexes:
- Low-impact exercise e.g., walking, recumbent exercise bike, or swimming.
- Strengthening exercises of legs and trunk to enhance postural stability.
- Gradual increase is essential to avoid fatigue or falls.
Integrating Measures for Maximum Effect
For optimal benefit, these measures need to be integrated together:
- Daily routines: Systematic morning mobilization, salt and fluid intake, compression application.
- Monitoring: Monitor symptoms and changes in blood pressure to make adjustments in interventions.
- Patient education: Educate patients to identify early warning signs of hypotension.
Case Example
A 65-year-old patient with AL amyloidosis and autonomic neuropathy developed dizziness on rising from bed:
- Employed gradual standing technique and leg-crossing maneuvers.
- Employed abdominal binder and knee-high compression stockings.
- Made adjustments in fluid and salt intake with physician supervision.
- Symptoms improved within 2 weeks, decreasing risk of falls.
This case demonstrates the utility of non-pharmacologic interventions in everyday life.
Conclusion
Non-pharmacological approaches have a key role to play in the management of orthostatic hypotension in amyloidosis. Important interventions are:
- Review and adjustment of medication
- Proper fluid and salt intake
- Gradual and cautious position changes
- Physical maneuvers enhancing venous return
- Head-of-bed elevation
- Compression garments
- Graded exercise
When applied on a regular basis, these interventions lessen symptoms, enhance functional capacity, and improve quality of life, sometimes in conjunction with pharmacologic treatment.
Key Takeaway:
Patient empowerment by using easily implemented, practical measures can effectively reduce the effects of orthostatic hypotension in systemic amyloidosis.

