Dietary Changes in Gastrointestinal Amyloidosis: Enhancing Symptoms and Nutrition
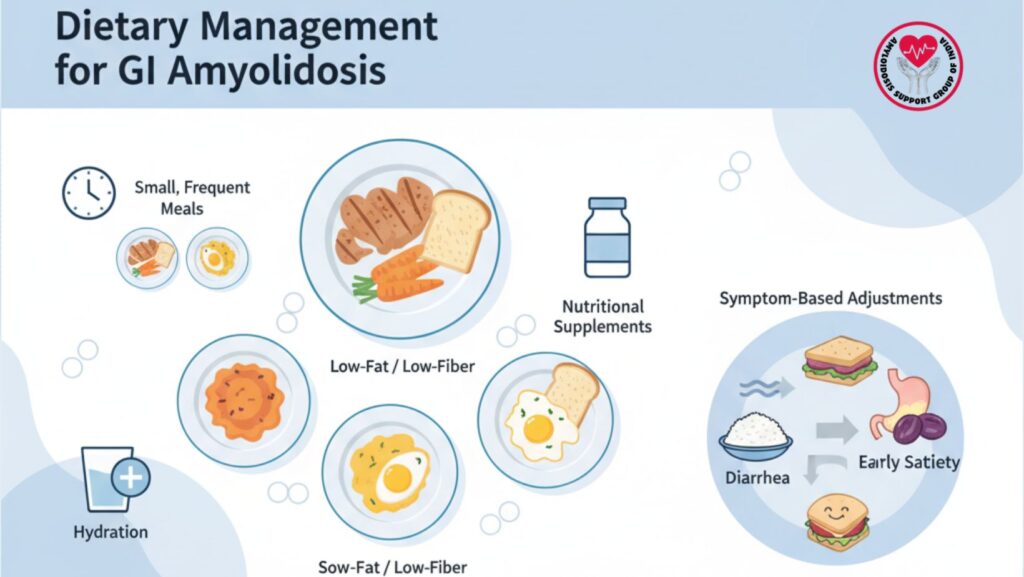
Table of Contents
Introduction
Systemic amyloidosis with GI involvement is an ubiquitous and problematic complication. Amyloidosis of the stomach, small intestine, and colon can interfere with motility, absorption, and digestion, resulting in early satiety, nausea, diarrhea, constipation, abdominal pain, and weight loss.
Nutrition is an indispensable aspect in controlling these symptoms, regulating body weight, and enhancing overall well-being. Symptom-specific dietary adjustments are required to maximize nutritional intake with the least GI distress.
This article is an exhaustive overview of dietary management techniques, effective meal planning, symptom-specific modifications, and additive nutritional interventions for GI amyloidosis patients.
1. Understanding GI Symptoms in Amyloidosis
1.1 Pathophysiology
- Amyloid deposits disrupt GI motility, absorption, and vascular integrity.
- Autonomic neuropathy is responsible for gastroparesis, diarrhea, and constipation.
- Vascular fragility and mucosal injury can exacerbate malabsorption and nutrient loss.
1.2 Common Symptoms Affecting Diet
- Early satiety: fullness after meals
- Weight loss: loss of appetite or malabsorption
- Nausea and vomiting: affects food tolerance
- Diarrhea: nutrient loss and dehydration
- Constipation: discomfort and lower appetite
2. Principles of Dietary Management
2.1 Small, Frequent Meals
- Consume 4–6 smaller meals rather than 2–3 large ones
- Reduces early satiety and bloating
- Encourages steady caloric intake during the day
2.2 Low-Fat Diet
- Fat delays gastric emptying and exacerbates nausea and early satiety
- Restrict high-fat foods: fried foods, heavy sauces, fatty meats
- Emphasize lean protein and healthy fats in small amounts
**2.3 Low Insoluble Fiber
- Insoluble fiber can worsen diarrhea or bloating
- Restrict raw vegetables, bran, whole grains if experiencing symptoms
- Opt for soluble fiber from oats, bananas, apples for mild constipation
2.4 Symptom-Based Modifications
- Diarrhea: restrict lactose, caffeine, and high-fructose foods
- Constipation: take in more fluid, soluble fiber, gentle exercise
- Nausea: consume bland, soft foods; avoid strong scent or spicy meals
- Early satiety: concentrate on high-calorie, nutrient-dense foods in small amounts
3. Meal Planning Strategies
3.1 Breakfast
- Banana or applesauce with small portion oatmeal
- Low-fat yogurt or soft scrambled eggs
- Dilitute juice or herbal tea
3.2 Mid-Morning Snack
- Almond milk, protein powder, and banana smoothie
- Small amount of nuts if well tolerated
3.3 Lunch
- Tofu, fish, or chicken as lean protein
- Vegetables cooked instead of raw
- Mashed potatoes, white rice, or pasta for comfort on the stomach
**3.4 Afternoon Snack
- Applesauce, rice cakes, or small protein shake
3.5 Dinner
- Baked fish or soft chicken
- Cooked carrots, zucchini, or squash
- Small serving of mashed sweet potatoes or rice
3.6 Evening Snack
- Low-fat yogurt or smoothie for added calories
4. Nutritional Supplementation
4.1 Oral Supplements
- High-calorie shakes and protein drinks for weight maintenance
- Enriched with vitamins and minerals to avoid deficiency
4.2 Enteral Nutrition
- For patients unable to take orally
- Nasogastric or PEG tube feeding can be employed in severe cases
4.3 Micronutrient Monitoring
- Iron, calcium, vitamin D, B12, and folate can be deficient
- Regular blood investigations to direct supplementation
5. Hydration Strategies
*
- Ensure adequate fluid intake to avoid dehydration, particularly with diarrhea
- Opt for water, herbal teas, broths, and electrolyte solutions
- Avoid carbonated or sugar-containing beverages if they exacerbate bloating or diarrhea
6. Managing Specific Symptoms Through Diet
6.1 Early Satiety
- Small meals, no liquids taken with meals
- High-calorie foods eaten between meals
- Restrict foods slowing gastric emptying
6.2 Diarrhea
- Low-fat, low-fiber diet
- Low-lactose or lactose-free dairy
- Probiotics for support of the gut microbiome
6.3 Constipation
- Sufficient fluids
- Soluble fiber foods
- Gentle exercise and regular timing of meals
6.4 Nausea and Vomiting
- Soft, bland foods
- Steer clear of greasy meals, spicy foods, or strong odors
- Peppermint or ginger can be calming
7. Role of Professional Support
7.1 Dietitian Consultation
- Adapt dietary plans to individual nutritional requirements and symptom patterns
- Regularly monitor intake, weight, and nutrient status
7.2 Multidisciplinary Care
- Consultation with gastroenterologists, hematologists, and primary care providers
- Combine dietary, pharmacologic, and systemic therapies for optimal results
8. Case Examples
Case 1: Early Satiety and Weight Loss
- 60-year-old patient with AL amyloidosis
- Intervention: small, frequent, high-calorie meals, low-fat diet
- Outcome: stabilized weight, less bloating, increased energy
Case 2: Diarrhea-Predominant Symptoms
- 58-year-old ATTR patient
- Intervention: low-fat, low-insoluble fiber diet, lactose-free products
- Outcome: fewer stools, better hydration, improved nutrition
9. Tips for Successful Dietary Management
- Monitor symptoms and meals to determine what triggers them
- Alcohol, fiber, and fat intake adjustment based on tolerance
- Utilization of nutrient-dense foods to keep calories in minimal amounts
- Addition of snacks and supplements to provide energy needs
- Informing patients and caregivers about food preparation and portioning
10. Monitoring and Follow-Up
Regular monitoring of weight, BMI, and body composition.
Monitoring of symptom response to diet changes.
Monitoring of laboratory markers for malnutrition or deficiency.
Diet adjustment based on disease progression and new symptoms
11. Integrating Diet with Medical Management
- Coordinate with medications for motility, diarrhea, or nausea
- Consider dietary adjustment with initiation of systemic amyloid therapies
- Remain flexible to alter meals based on tolerance and GI function
12. Emerging Nutritional Approaches
- Prebiotics and probiotics for gut microbiota health
- Anti-inflammatory diets to minimize GI irritation
- Utilization of functional foods and nutrient-fortified products
- Investigation of personalized nutrition in amyloidosis to enhance outcomes
13. Patient Education
- Highlight importance of small, frequent meals
- Teach on identification of food triggers for diarrhea or bloating
- Encourage monitoring intake and symptoms for modification
- Offer advice on supplements and fluid intake
- Involve caregivers in food planning and preparation
14. Conclusion
Dietary adjustments are central to gastrointestinal symptom management in systemic amyloidosis. Essential measures include:
- Small, frequent meals to counteract early satiety
- Low-fat and low-insoluble fiber diet to minimize diarrhea and bloating
- Tolerance-based adjustments that are symptom-based
- Supplemental nutrition and hydration to ensure energy and avoid malnutrition
Optimal nutrition, symptom management, and quality of life are achieved through a multidisciplinary care model that includes dietitians, gastroenterologists, and systemic amyloidosis specialists. Ongoing monitoring, patient education, and adaptation of dietary planning are crucial for chronic disease management.

