Table of Contents
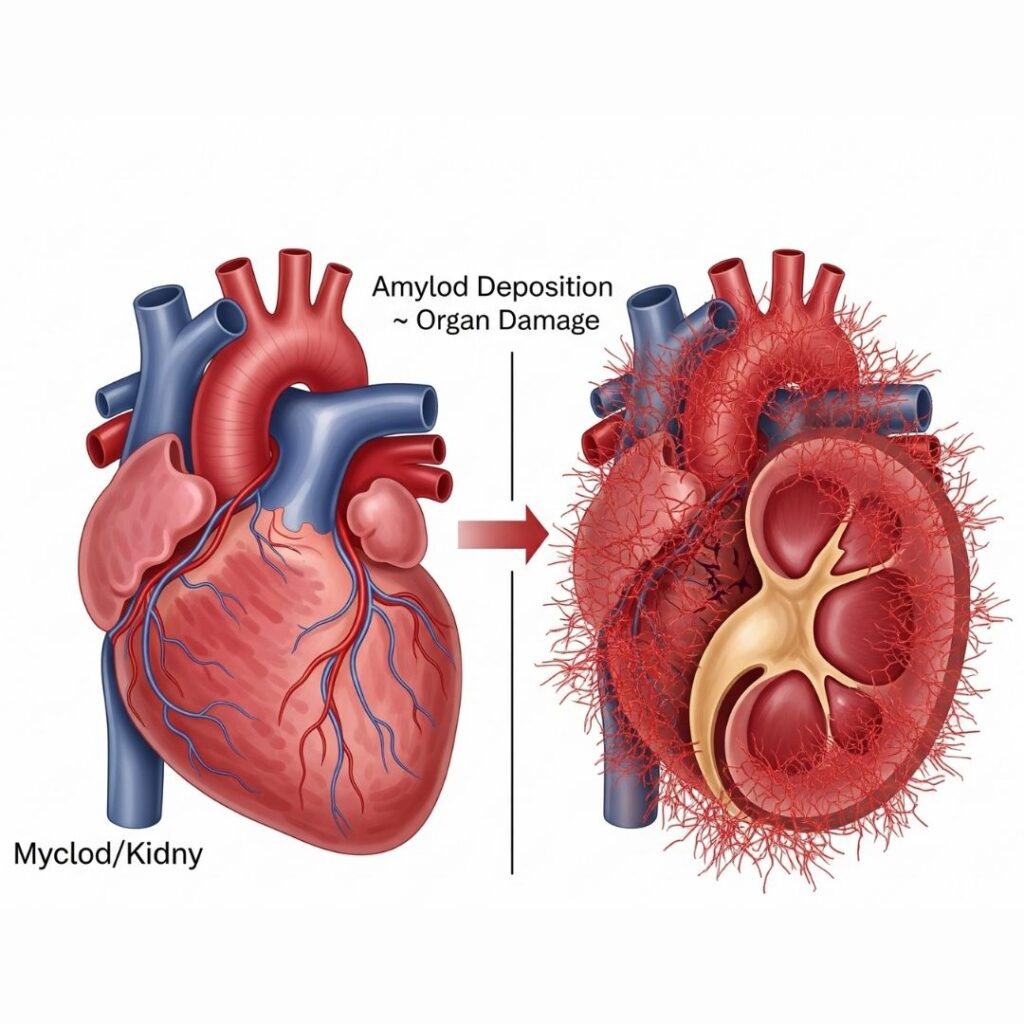
Introduction-Amyloid Deposition Cause Organ Damage
Amyloidosis is a multifaceted and poorly appreciated class of diseases resulting from aberrant deposits of a protein known as amyloid. The deposits can appear in an array of tissues and organs and result in marked dysfunction and, in the worst cases, organ failure. But how does amyloid deposition lead to damage at the cellular and organ levels?
This comprehensive article will delve into the biological process of amyloid formation, how it becomes a disruptor to organ function, and the long-term consequences of this disease. As a patient, caregiver, or just interested in learning more, you can learn more about this subject and better understand the severity of amyloidosis and the necessity for early detection and help.
What Is Amyloidosis?
Amyloidosis is a rare yet severe disorder in which amyloid proteins accumulate in the tissues and organs. These proteins are typically misfolded and become insoluble fibrils that the body cannot effectively degrade or eliminate.
There are various forms of amyloidosis, such as:
- AL (Primary) Amyloidosis – associated with plasma cell disorders such as multiple myeloma.
- AA (Secondary) Amyloidosis – commonly results from chronic infection or inflammatory illnesses.
- ATTR Amyloidosis – resulting from mutations in the transthyretin (TTR) gene.
- Hereditary Amyloidosis – inherited through generations.
- Dialysis-related Amyloidosis – linked to dialysis therapy lasting several years.
Understanding Amyloid Proteins and Their Formation
Proteins in the human organism typically fold into specific three-dimensional structures so that they can carry out their functions normally. Under some conditions, though—like genetic mutations, chronic inflammation, or aging—proteins can misfold and clump together into amyloid fibrils.
How Amyloid Fibrils Form
- Protein Misfolding: Soluble proteins unfold and reveal hydrophobic patches.
- Oligomer Formation: The misfolded proteins aggregate to create small groups (oligomers).
- Fibril Aggregation: The oligomers assemble into long, insoluble fibrils.
- Tissue Infiltration: These fibrils are deposited in organs and tissues.
Where Does Amyloid Deposit in the Body?
Amyloid deposit can occur in nearly every organ, but most commonly affected organs include:
- Heart
- Kidneys
- Liver
- Spleen
- Nervous system
- Digestive tract
- Skin
Different organs respond in different ways to amyloid deposition, and that is why symptoms may be so diverse.
Mechanisms of Organ Damage from Amyloid Deposition
1. Disruption of Cellular Architecture
Amyloid deposits substitute the structure of normal tissues, resulting in the loss of cellular function. For instance:
- In the heart, heart muscles are infiltrated by amyloid, resulting in stiffness (restrictive cardiomyopathy) and decreased pumping efficiency.
- In the kidneys, amyloid accumulates in glomeruli, diminishing their capacity to filter blood, resulting in proteinuria and renal failure.
2. Compression of Blood Vessels
Amyloid can compress small blood vessels (capillaries), limiting oxygen and nutrient supply to tissues. This causes ischemia and tissue injury over time.
3. Inflammation and Oxidative Stress
Amyloid fibrils tend to induce immune reactions. The emission of inflammatory cytokines and reactive oxygen species (ROS) leads to tissue injury and cell death.
4. Loss of Elasticity in Tissues
Tissues like the liver or spleen may swell and harden as a result of amyloid deposition. Their capacity to undertake their usual physiological functions is impaired.
5. Nerve Damage
In neuropathic amyloidosis (such as familial ATTR), amyloid accumulates around the nerve cells, interfering with signal transmission and producing symptoms that include:
- Numbness
- Tingling
- Loss of motor control
- Autonomic dysfunction
Damage Caused to Organs Due to Amyloid Deposition
A. Heart (Cardiac Amyloidosis)
Amyloid infiltrates the myocardium, resulting in:
- Thickened walls with decreased elasticity
- Diastolic dysfunction
- Arrhythmias
- Congestive heart failure
- Sudden cardiac arrest in advanced disease
B. Kidneys (Renal Amyloidosis)
Amyloid replaces normal glomerular structures:
- Results in nephrotic syndrome
- Proteinuria (excess protein in urine)
- Leg and ankle swelling
- Progressive renal failure
C. Liver and Spleen
Amyloid deposition results in:
- Hepatomegaly (liver enlargement)
- Increased liver enzymes
- Portal hypertension
- Splenomegaly
D. Nervous System
Peripheral and autonomic nervous systems are injured:
- Loss of motor function and sensation
- Instability of blood pressure
- Gastrointestinal symptoms (gastroparesis, diarrhea)
- Erectile dysfunction
E. Digestive System
Gastrointestinal amyloidosis can result in:
- Diarrhea or constipation
- Bruising from fragile blood vessels
- Malabsorption of nutrients
- Weight loss
F. Skin and Soft Tissue
Occasionally, amyloid deposited in the skin causes:
- Waxy, shiny patches
- Easily bruised skin
- Purpura, particularly around the eyes
Amyloidosis Organ Damage Symptoms
The symptoms of amyloidosis are mimicked by many other conditions, and for this reason, amyloidosis is frequently misdiagnosed. Frequent evidence of organ damage includes:
- Fatigue
- Shortness of breath
- Leg or abdominal swelling
- Numbness or tingling of limbs
- Unintended weight loss
- Irregular heartbeats
- Foamy or dark urine
- Enlarged tongue (macroglossia)
Diagnostic Strategies
To diagnose amyloidosis and determine organ damage:
1. Biopsy
Tissue sample stained with Congo red dye to detect amyloid under polarized light.
2. Blood and Urine Tests
Check for abnormal proteins (such as light chains in AL amyloidosis).
3. Imaging
- Echocardiogram
- MRI
- Scintigraphy (bone scans to identify cardiac ATTR)
4. Genetic Testing
In hereditary amyloidosis.
Treatment Options: Reducing Amyloid Burden and Protecting Organs
A. Targeting Underlying Causes
- AL Amyloidosis: Chemotherapy to decrease plasma cells.
- ATTR Amyloidosis: Stabilizers such as Tafamidis or gene-silencing agents such as Patisiran.
B. Organ-Specific Management
- Diuretics for heart failure
- ACE inhibitors to protect kidneys
- Pain relief medication for neuropathy
- Dietary modifications for GI symptoms
C. Transplants
- Liver transplant in hereditary ATTR
- Heart/kidney transplant in advanced cases
D. Supportive Care
- Physical therapy
- Nutritional counseling
- Pain management
- Regular monitoring
Importance of Early Diagnosis
Early identification can:
- Slow down disease progression
- Improve quality of life
- Delay or prevent organ failure
- Enhance response to treatment
Raising awareness is important to catching the disease in its earlier, more treatable stages.
Living with Organ Damage from Amyloidosis
Though amyloidosis is a life-changing disease, numerous patients have normal lives through:
- Regular medical follow-up
- Dietary and lifestyle changes
- Mental and emotional well-being support
- Involvement in clinical trials
Amyloidosis Support Communities’ Role
Patient support groups and advocacy websites such as amyloidosissupport assist by:
- Relating real experiences and anecdotes
- Providing access to specialist information
- Bringing patients and caregivers together
- Promoting awareness for early diagnosis
Conclusion
Amyloid deposition is an insidious process that quietly but tenaciously derails organ function. By learning how it happens—from protein misfolding to replacement of normal tissues—patients and doctors can work together more effectively to diagnose, treat, and care for individuals impacted.
If you or a loved one is being confronted with a possible diagnosis, keep in mind: Knowledge is power, and early action has the potential to be life-altering.

