How is Amyloidosis Diagnosed?
Table of Contents
Amyloidosis is a rare but potentially fatal condition in which abnormal protein, known as amyloid, accumulates in organs and tissues. Because of its nonspecific presentation and mimicry of other diseases, precisely diagnosing amyloidosis can prove difficult. Yet, the development of new diagnostic technologies and increased awareness have enhanced the diagnostic process.
In this detailed guide, we’ll explore how amyloidosis is diagnosed, the tests and techniques involved, the significance of Congo red staining, and why early diagnosis is crucial for managing this potentially life-threatening condition.
1. Introduction to Amyloidosis
Amyloidosis is a set of diseases due to the extracellular deposition of amyloid fibrils—abnormal protein aggregates—in organs and tissues. Such deposits can disrupt normal organ function, most notably in the heart, kidneys, liver, nerves, and gastrointestinal tract.
There are various forms of amyloidosis, such as:
- AL (Primary) Amyloidosis – associated with plasma cell disorders
- AA (Secondary) Amyloidosis – linked with chronic inflammatory diseases
- ATTR Amyloidosis – associated with a mutation in the transthyretin (TTR) gene
- Aβ2M Amyloidosis – frequent in dialysis patients
Each has its own specific diagnostic and treatment protocol.
2. Importance of Early Diagnosis
Early diagnosis is critical for two reasons:
- Prevention of irreversible organ damage
- Initiation of targeted therapies
Delayed diagnosis usually leads to severe organ dysfunction, mainly of the heart and kidneys, which can dramatically influence the patient’s quality of life and prognosis.
3. Symptoms Leading to Clinical Suspicion
Despite the multitude of symptoms caused by amyloidosis, its symptoms are non-specific and organ-specific. Below are some red flags that can lead a physician to suspect amyloidosis:
Common Signs & Symptoms:
- Unexplained weight loss
- Fatigue
- Leg or ankle swelling (if the kidney or heart is involved)
- Shortness of breath
- Tingling or numbness (peripheral neuropathy)
- Swelling of the tongue (macroglossia)
- Bruising easily around the eyes (periorbital purpura)
- Constipation or diarrhea
Since these symptoms overlap with those of other diseases, amyloidosis usually remains undetected until extensive damage has been done.
4. Initial Laboratory Tests
Physicians will usually start by taking normal blood and urine tests to evaluate organ function and search for abnormalities.
Basic Investigations:
- Complete Blood Count (CBC)
- Comprehensive Metabolic Panel (CMP)
- Serum creatinine and BUN (Kidney function)
- Liver function tests
- Serum and urine protein electrophoresis (SPEP/UPEP)
Unusual protein bands on SPEP or UPEP can indicate the presence of monoclonal light chains—frequently encountered in AL amyloidosis.
5. Biopsy: The Cornerstone of Diagnosis
The tissue biopsy is the gold standard to establish amyloid deposits.
Types of Biopsy:
- Abdominal fat pad aspiration (less invasive)
- Bone marrow biopsy (in suspected AL amyloidosis)
- Organ-specific biopsies (kidney, heart, liver, or rectum)
Biopsy tissues are usually stained with Congo red, which is important for identifying amyloid.
6. Congo Red Staining Explained
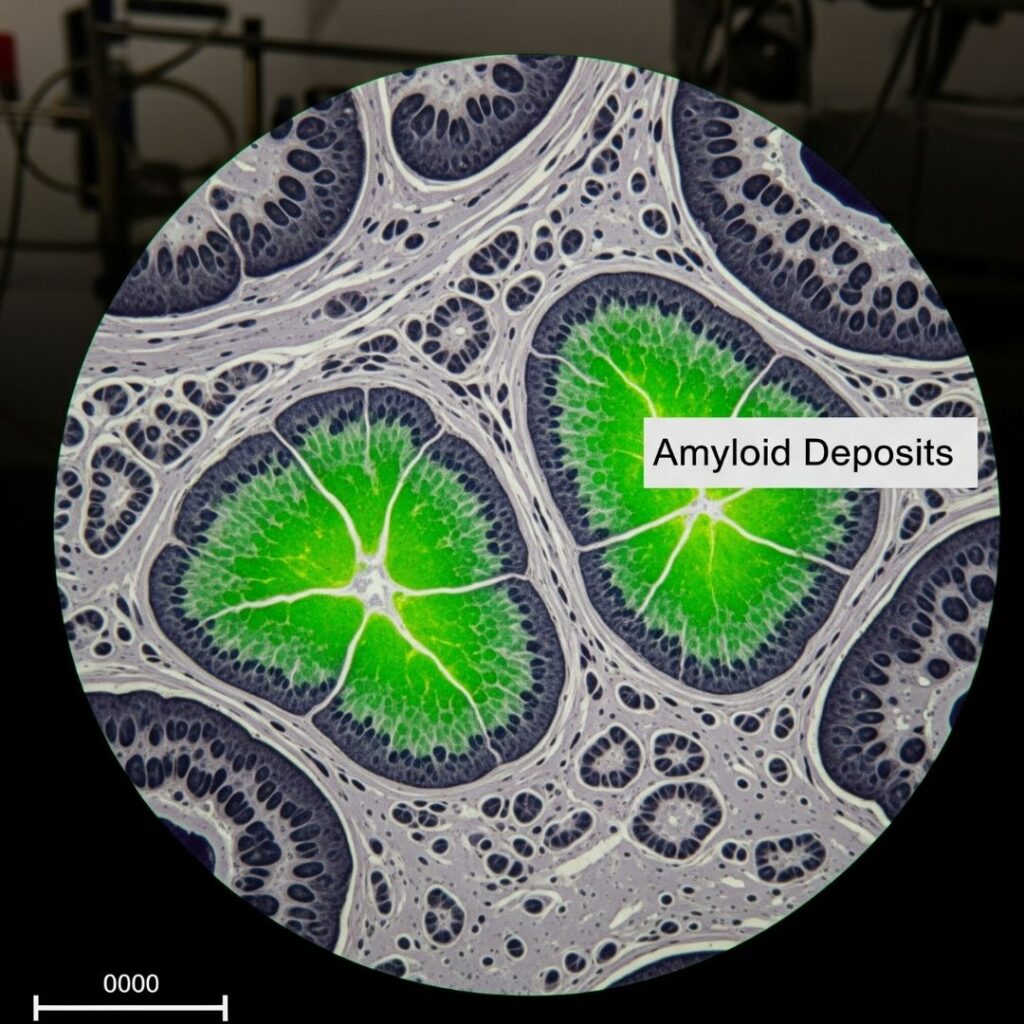
Congo red staining is a specific histological stain that detects amyloid deposits.
Key Features:
- Under normal light: Amyloid is pink-red
- Under polarized light: Exhibits apple-green birefringence, diagnostic of amyloid
This apple-green birefringence is the gold standard confirmation of amyloidosis.
7. Advanced Imaging Techniques
Imaging aids in evaluating organ involvement, particularly the heart.
Echocardiography:
- Thickened walls of the heart with “sparkling” appearance
- Decreased heart function
Cardiac MRI:
- Aids in distinguishing amyloidosis from other cardiomyopathy causes
Nuclear Imaging:
- Technetium-99m pyrophosphate (PYP) scan assists in detecting ATTR amyloidosis
- Useful in evading cardiac biopsy
8. Blood and Urine Testing
To test for AL amyloidosis, tests target the detection of free light chains and monoclonal proteins.
Key Tests:
- Serum Free Light Chain Assay
- Serum and Urine Immunofixation Electrophoresis (IFE)
- Bence-Jones proteins in urine
These tests identify the clonal plasma cell disorder behind AL amyloidosis.
9. Genetic Testing for Hereditary Amyloidosis
For suspected hereditary (ATTRm) amyloidosis, a genetic test is required.
What It Entails:
- DNA testing for mutations in the TTR gene
- Assists in differentiating ATTRm (mutant) from ATTRwt (wild-type) amyloidosis
Family members might also be benefited with testing if a mutation is identified.
10. Subtyping Amyloidosis: Why It Matters
Accurate identification of the type of amyloidosis is important because there are different treatments.
Subtyping Techniques:
- Immunohistochemistry (IHC)
- Mass spectrometry-based proteomic analysis
- Laser microdissection with mass spectrometry (LMD-MS) – gold standard for subtyping
Without accurate subtyping, patients can be treated with ineffective or even toxic treatment.
11. Multidisciplinary Diagnosis Approach
Diagnosis of amyloidosis may involve collaboration from:
- Hematologists
- Cardiologists
- Nephrologists
- Pathologists
- Neurologists
- Genetic counselors
This multidisciplinary process guarantees an accurate diagnosis and targeted treatment regimen.
12. Diagnosis Challenges
Despite progress, amyloidosis is still challenging to diagnose because:
- Rarity and low physician awareness
- Features shared with other diseases
- Misdiagnosis for heart failure, nephrotic syndrome, or neuropathy
- Inadequate access to advanced diagnostic equipment in some areas
Early diagnosis and specialist referral are the priority.
13. Case Studies & Real-World Insights
Case 1: Delayed Diagnosis in AL Amyloidosis
A 52-year-old man had fatigue, weight loss, and swelling. Months of being misdiagnosed as kidney disease followed before a kidney biopsy disclosed Congo red positive amyloid deposits. Subsequent testing showed AL amyloidosis.
Lesson: Early biopsy and high clinical suspicion are the takeaway.
Case 2: ATTR Cardiac Amyloidosis Identified via PYP Scan
An 80-year-old male patient with inexplicable heart failure was scanned for PYP, which showed uptake indicative of ATTRwt. Genetic testing excluded mutation.
Lesson: Imaging can minimize the requirement for biopsy.
14. FAQs
Q1: What is the most definitive test for amyloidosis?
A: Congo red staining of a biopsy specimen, demonstrating apple-green birefringence under polarized light, is diagnostic.
Q2: Can amyloidosis be detected through blood tests?
A: Light chains or abnormal proteins can be detected by blood tests, but usually a biopsy is required for confirmation.
Q3: Is genetic testing required for all patients?
A: Only when there is suspected hereditary ATTR amyloidosis or a family history.
Q4: Which organs are most frequently biopsied?
A: Fat pad, kidney, bone marrow, heart, and liver based on symptoms.
15. Conclusion
Amyloidosis is a subtle, multifaceted illness that demands a high index of clinical suspicion and a systematic approach to diagnosis. From laboratory studies of the blood and urine to Congo red staining and advanced imaging techniques, every step is important in determining not just the occurrence of amyloid but also its nature and degree of organ involvement.
The early and accurate diagnosis of amyloidosis can significantly improve prognosis, prevent irreversible damage, and guide targeted therapy. If symptoms suggest amyloidosis, it’s essential to consult specialists experienced in rare diseases and consider referral to a center of excellence.

