Atrial Fibrillation in Cardiac Amyloidosis: Prevalence, Risks, and Management
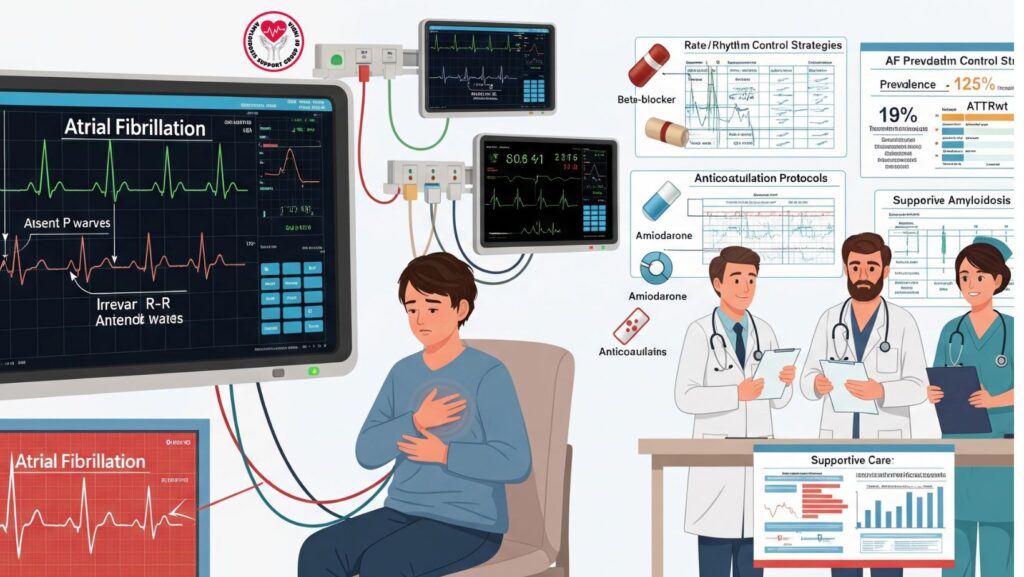
Table of Contents
1. Introduction
Atrial fibrillation (AF) is a frequent arrhythmia in cardiac amyloidosis (CA), especially in wild-type transthyretin (ATTRwt) amyloidosis patients. AF is responsible for symptom burden, worsening of heart failure, thromboembolic risk, and decreased quality of life.
Knowledge of the prevalence, pathophysiology, clinical impact, and management strategies of AF in CA is crucial for clinicians and supportive care teams.
2. Prevalence of Atrial Fibrillation in Cardiac Amyloidosis
- AF prevalence in CA varies between 10% and 69% based on subtype and population studied.
- ATTRwt amyloidosis: most frequently linked with AF through age-related atrial remodeling and amyloid deposition.
- ATTRv amyloidosis: reduced prevalence, depending on mutation and phenotype.
- AL amyloidosis: moderate AF prevalence; may present with advanced cardiac disease.
Clinical implication: AF occurs more often in patients with older age, larger atria, left ventricular hypertrophy, and diastolic dysfunction.
3. Pathophysiology of AF in CA
- Amyloid deposit in atria: results in atrial stiffness, fibrosis, and conduction disturbances
- Increased atrial pressures: are the result of ventricular diastolic dysfunction, leading to dilation of atria
- Autonomic dysfunction: especially in AL amyloidosis with neuropathy
- Inflammation and microvascular ischemia: play a role in arrhythmogenic substrate
Outcome: These conditions generate a pro-arrhythmic setting, enhancing the risk of both paroxysmal and persistent AF.
4. Clinical Impact and Complications
- Exacerbation of heart failure: atrial kick loss accentuates diastolic filling in rigid ventricles
- Risk of thromboembolism: enhanced risk of stroke and systemic embolism, even when in sinus rhythm, due to atrial impairment
- Symptoms: palpitations, fatigue, shortness of breath, syncope
- Hospitalizations: AF is responsible for readmission in CA patients
Key point: AF management is crucial for symptom control, hemodynamic stability, and stroke prevention.
5. Diagnosis of AF in Cardiac Amyloidosis
- Electrocardiogram (ECG): first-line for AF detection
- Holter monitoring: for paroxysmal or asymptomatic AF
- Echocardiography: assesses atrial size, diastolic function, and thrombus risk
- Advanced imaging (Cardiac MRI/CT): can evaluate atrial fibrosis and amyloid burden
6. Management Strategies
6.1 Rate Control
- Preferred in most CA patients because of tolerance problems with negative inotropes
- Beta-blockers: can decrease cardiac output, use with caution
- Calcium channel blockers: usually avoided in AL amyloidosis because of sensitivity
- Digoxin: use with caution; amyloid myocardium is sensitive, can trigger toxicity
6.2 Rhythm Control
- Consider in symptomatic, hemodynamically unstable, or recently diagnosed patients
Amiodarone is preferred for CA because of minimal negative inotropic effects
- Catheter ablation: limited evidence; might benefit some ATTR patients with paroxysmal AF
6.3 Anticoagulation
- High thromboembolic risk despite preserved LVEF
- Apply CHA₂DS₂-VASc scoring cautiously; numerous experts prefer anticoagulation for all CA patients with AF
- Choose: warfarin or direct oral anticoagulants (DOACs) according to renal function
6.4 Supportive Care Integration
- Maximize heart failure management (loop diuretics, SGLT2 inhibitors, GDMT if tolerated)
- Check volume status, BP, renal function
- Education of patients regarding symptom identification, stroke warning signs, and compliance
7. Special Considerations in ATTR vs AL Amyloidosis
- ATTRwt: elderly patients, greater prevalence of AF, rhythm control potentially more possible
- AL amyloidosis: frequently sicker, frail, hypotensive-prone; rate control preferred
- Disease-specific therapy: tafamidis, RNA therapies, or chemotherapy can decrease amyloid burden and enhance atrial remodeling
8. Monitoring and Follow-up
- Routine ECGs and Holter monitoring
- Echocardiography to measure atrial size and function
- Biomarkers: NT-proBNP, troponin for heart failure evaluation
- Symptoms reported by the patient: palpitations, fatigue, dyspnea
Objective: Early diagnosis of AF, adjustment of treatment, and prevention of complications.
9. Prognosis and Outcomes
- AF is characterized by poorer prognosis in CA because of:
- Greater hospitalizations for heart failure
- Increased thromboembolic events
- Increased symptom burden
- Optimal care can enhance quality of life and prevent complications
10. Case Example (Optional)
A 72-year-old patient with ATTRwt cardiac amyloidosis:
- History: NYHA class II symptoms, fatigue, intermittent palpitations
- ECG: paroxysmal AF
- Treatment: low-dose beta-blocker for rate control, anticoagulation with DOAC, loop diuretic for volume, tafamidis therapy
- Result: Stable heart rate, improved symptoms, no thromboembolic events
11. Conclusion
Atrial fibrillation is frequent in cardiac amyloidosis, particularly ATTRwt, and has important effects on symptoms, heart failure, and thromboembolic risk.
Key Takeaways:
- Prevalence: 10% to 69%, highest for ATTRwt
- Treatment involves rate/rhythm control, anticoagulation, and supportive care
- Multidisciplinary management enhances safety, symptom control, and quality of life
- Early diagnosis and treatment are important for preventing complications

