Case Report: Abdominal CT Findings in a 61-Year-Old Patient – Ascites and Possibly Nodular Liver
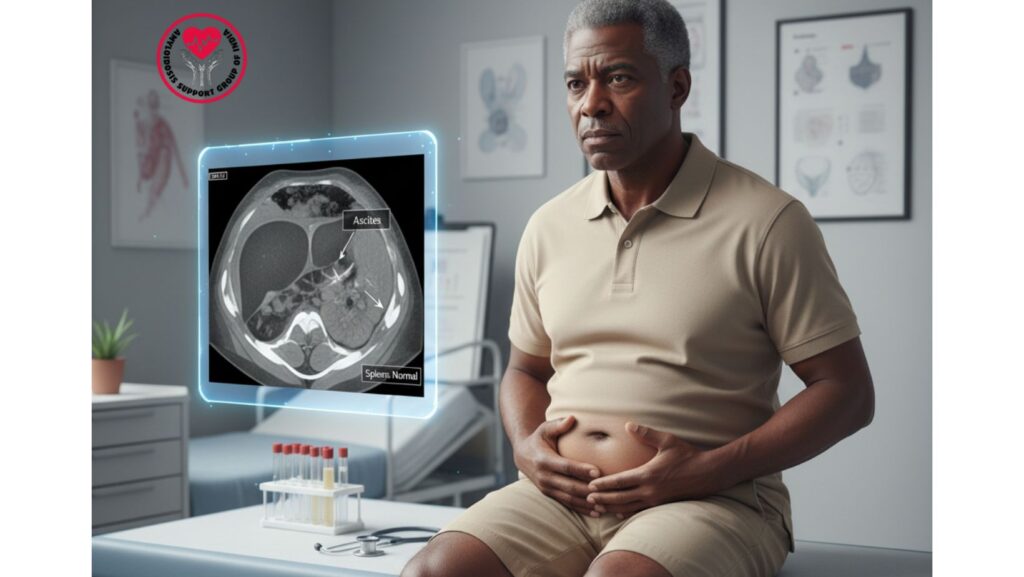
Table of Contents
Introduction
Abdominal imaging is an important evaluation tool for patients with edema, ascites, and liver enzyme abnormality. Computed tomography (CT) yields high-anatomical detail, allowing clinicians to detect ascites, liver morphology, and other intra-abdominal pathology.
In this instance, a 61-year-old African-American man presented with progressive swelling of the legs and abdominal distension. An abdominal CT scan showed ascites and possibly nodular liver without hepatosplenomegaly, yielding information on hepatic involvement, progression of systemic disease, and differential diagnosis.
Patient Profile
*
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Relevant Medical History: Hypertension, mild diabetes
- Presenting Symptoms: Bilateral leg swelling, abdominal distension, fatigue
Clinical Presentation
The patient complained:
- Progressive bilateral leg swelling (edema)
- Abdominal distension (ascites)
- Fatigue and weakness
- Early satiety and mild weight loss
- Shortness of breath on exertion
Physical Examination Findings: - Pitting edema of lower extremities
- Tense ascites with positive fluid wave
- Jugular venous distention
- Mild hepatomegaly
- No jaundice or signs of acute liver failure
Laboratory Findings
*
- Albumin: 2.1 g/dL (low)
- Total Bilirubin: 0.5 mg/dL
- Alkaline Phosphatase: 718 IU/L
- AST: 158 IU/L
- ALT: 119 IU/L
- INR: 1.07
- Creatinine: 0.9 mg/dL
- Nephrotic-range proteinuria
- Viral and autoimmune tests: Normal
- Serum Protein Electrophoresis (SPEP): Normal
Abdominal CT Scan Findings
- Ascites: Moderate fluid in peritoneal cavity
- Liver: Possibly nodular in appearance
- Spleen: Normal size (no hepatosplenomegaly)
- Other Organs: Kidneys, pancreas, and bowel loops showed no remarkable findings
- No mass lesions, biliary obstruction, or portal vein thrombosis
Interpretation of CT Findings
1. Ascites
- Establishes clinical suspicion based on physical exam.
- Etiology can be:
- Hypoalbuminemia caused by nephrotic-range proteinuria
- Portal hypertension due to liver disease
- Cardiac causes (right-sided heart failure in restrictive cardiomyopathy)
2. Possibly Nodular Liver
- Implicates early hepatic structural changes, which can be:
- Regenerative nodules secondary to chronic liver injury
- Infiltrative processes like amyloidosis
- Lack of hepatosplenomegaly suggests preservation of liver size, decreasing probability of advanced cirrhosis.
3. Lack of Hepatosplenomegaly
- Excludes severe portal hypertension, congestive hepatopathy, or extensive infiltrative disease.
- Consistent with early or mild hepatic involvement, as it corresponds with normal INR and bilirubin.
Clinical Significance
- Advances Multi-Organ Assessment
- Imaging aids laboratory results (normal bilirubin, INR) and assists in detecting subclinical liver involvement.
- Informs Differential Diagnosis
- Nodular liver without hepatosplenomegaly diminishes suspicion for cirrhosis, chronic viral hepatitis, or congestive hepatopathy.
- Facilitates systemic infiltrative disease such as amyloidosis or early fibrosis.
- Therapeutic Planning
- Maintained liver morphology and function permit safe chemotherapy administration or other systemic treatment.
- Time course of liver nodularity aids in evaluating disease progression.
Diagnostic Correlation
- Systemic Amyloidosis Suspected:
- Multi-organ symptoms: edema, ascites, proteinuria, mild elevation of liver enzymes
- Lab correlation: normal viral and autoimmune panels, hypoalbuminemia, nephrotic-range proteinuria
- Imaging: ascites, potentially nodular liver, no hepatosplenomegaly
- Supporting Diagnostics:
- Fat pad biopsy: Congo red positive for amyloid deposits
- Renal biopsy: confirmed glomerular amyloidosis
- Cardiac evaluation: restrictive cardiomyopathy
Management
Supportive Care
- Diuretics for edema and ascites
- Salt restriction and fluid management
- Nutritional support to correct hypoalbuminemia
Disease-Specific Therapy
- Chemotherapy: CyBorD regimen (Bortezomib, Cyclophosphamide, Dexamethasone)
- Stem Cell Transplantation for candidates
- Novel therapies: Daratumumab in refractory amyloidosis
Monitoring
- Serial abdominal imaging to check liver morphology and ascites
- Liver function tests (LFTs) such as bilirubin, AST, ALT, AP
- Renal function and urine protein
- Cardiac assessment for restrictive cardiomyopathy
Patient Outcome
*
- After 6 months:
- Ascites significantly improved with diuretics
- Nodular appearance of the liver remained stable; no hepatosplenomegaly developed
- Liver enzymes trended downward
- Renal function was preserved, proteinuria modestly decreased
- Overall quality of life improved
Clinical Insights
For Clinicians
- Abdominal CT offers useful structural information to augment labs in systemic disease.
- Ascites in combination with potentially nodular liver but no hepatosplenomegaly implies early hepatic involvement.
- Directs treatment safety and prognosis evaluation.
For Patients & Families
- CT findings are useful in explaining involvement of organs without reflecting on severe liver injury.
- Early detection and treatment enhance outcome over the long term.
- Continuous monitoring is essential in detection of disease progression.
Broader Implications
*
- Imaging must be combined with lab work, clinical presentation, and biopsy findings.
- Subtle nodularity and early structural change may reflect systemic infiltrative disease.
- Avoids misdiagnosis and directs appropriate therapy in multi-organ conditions such as amyloidosis.
Conclusion
The abdominal CT scan of this 61-year-old patient yielded:
- Ascites, verifying fluid accumulation
- Potentially nodular liver, indicating incipient hepatic alterations
- No hepatosplenomegaly, showing maintained organ size
These findings, combined with normal viral/autoimmune workup and other tests, assisted clinicians to rule out primary liver disease and concentrate on systemic amyloidosis.
Key Takeaway: Imaging is a key instrument in assessing systemic disease, directing diagnosis, treatment, and prognosis, even when laboratory values are mildly abnormal.

