CNS Complications in ATTRv Amyloidosis: Leptomeningeal Amyloidosis and Neurological Manifestations
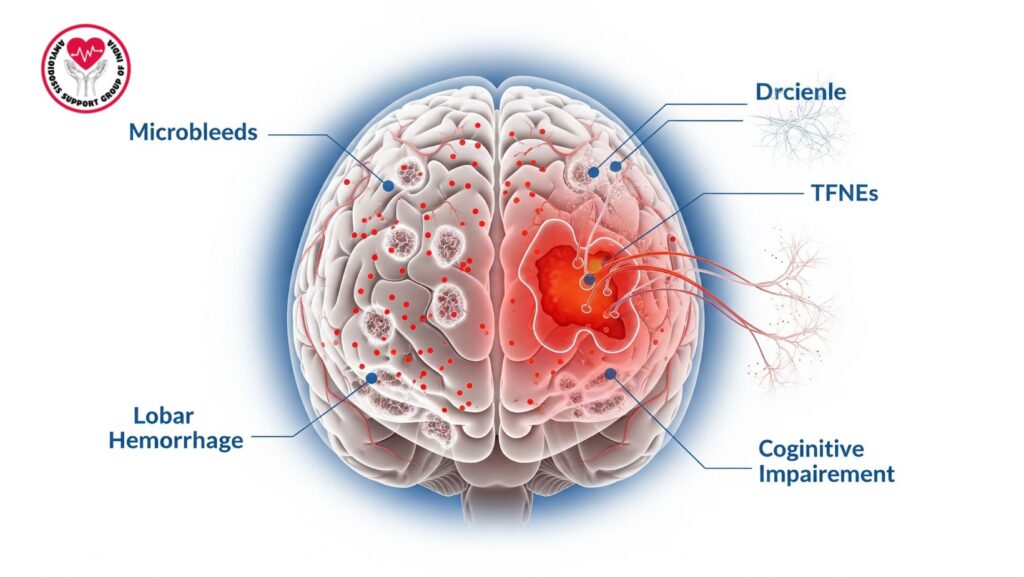
Table of Contents
Introduction
Amyloidosis is a disparate group of disease conditions due to the deposition of misfolded protein fibrils outside the cell. Of these, hereditary transthyretin amyloidosis (ATTRv) is a rare yet clinically important disorder, due to mutations in the transthyretin (TTR) gene. ATTRv can manifest as polyneuropathy, cardiomyopathy, and ocular involvement but has an underappreciated and severely disabling feature of central nervous system (CNS) involvement.
CNS manifestations in ATTRv are largely the result of leptomeningeal amyloidosis (LA), with deposits of amyloid in leptomeningeal vessels and tissues. In contrast to systemic deposition, CNS manifestations are exclusive to ATTRv since the brain is protected from circulating amyloidogenic TTR by the blood–brain barrier but mutant TTR produced locally in the choroid plexus and retina can penetrate local structures.
This paper discusses extensively the pathophysiology, clinical presentation, diagnostic difficulties, and management of CNS complications in ATTRv amyloidosis, with emphasis on leptomeningeal amyloidosis.
Pathophysiology of CNS Involvement in ATTRv
Why CNS Is Affected in ATTRv
- The choroid plexus secretes TTR, which is carried in cerebrospinal fluid (CSF).
- Mutant TTR aggregates in leptomeningeal vessels and meninges.
- Deposits lead to vascular fragility, microbleeds, and neuronal dysfunction.
Mechanisms Leading to Complications
- Vascular amyloid deposition: Weakening of vessel walls, with risk of lobar hemorrhages.
- Tissue infiltration: Direct compression and malfunctioning of cortical and subcortical neurons.
- Neurotoxicity of oligomers: Disrupts synaptic function, causing cognitive deterioration.
CNS Complications in ATTRv Amyloidosis
1. Cerebral Microbleeds
- Small, asymptomatic hemorrhagic lesions on MRI (susceptibility-weighted imaging).
- Representative of fragile amyloid-filled vessels.
- Frequently multiple and in cortical or subcortical areas.
2. Lobar Hemorrhages
- Symptomatic brain bleeds in cortical lobes.
- Can present with acute headache, focal deficits, or seizures.
- May recur, leading to progressive disability.
3. Transient Focal Neurological Episodes (TFNEs)
- Sudden, short-lived neurological symptoms (e.g., weakness, sensory loss, speech arrest, visual phenomena).
- Mimic transient ischemic attacks but are caused by cortical irritation from superficial bleeds.
- Often a warning sign of advanced leptomeningeal involvement.
4. Cognitive Impairment
- Progressive impairment of memory, executive function, and processing speed.
- Concurrent with cumulative vascular injury and direct amyloid neurotoxicity.
- Can mimic vascular dementia or Alzheimer’s disease.
5. Other Manifestations
- Meningeal irritation headache.
- Seizure due to cortical involvement.
- Ataxia or gait impairment due to cerebellar microhemorrhages.
Epidemiology and Genetic Aspects
- CNS involvement most commonly reported in late-onset ATTRv mutations, including Val30Met (non-endemic regions), Tyr114Cys, and Leu12Pro.
- Symptoms occur many decades following onset of peripheral neuropathy or cardiomyopathy.
- Genetic testing and family history are still crucial for early diagnosis.
Diagnosis of CNS Amyloidosis in ATTRv
Neuroimaging
- MRI with SWI or GRE sequences → shows microbleeds, superficial siderosis, and hemorrhages.
- FLAIR imaging → reveals leptomeningeal thickening.
CSF Analysis
- Can show increased protein or TTR variants.
- Not routinely diagnostic but supportive.
Histopathology
- Seldom performed, but biopsy/autopsy reveals amyloid deposits in leptomeningeal vessels.
Neurocognitive Testing
- Reveals subtle executive dysfunction and memory impairment.
Differential Diagnosis
- Cerebral amyloid angiopathy (CAA) secondary to Aβ amyloid.
- Alzheimer’s disease.
- Vascular dementia due to other small vessel diseases.
Management of CNS Complications in ATTRv
Disease-Modifying Therapies
- Existing systemic ATTRv treatments (tafamidis, patisiran, inotersen, vutrisiran) are limited in CNS penetration by virtue of the blood–brain barrier.
- CNS-penetrant therapies are being researched to develop (e.g., intrathecal antisense oligonucleotides).
Symptomatic Management
- Hemorrhage Control
- Routine stroke management protocols.
- Anticoagulants/antiplatelet avoidance when feasible.
- TFNEs
- Cortical hyperexcitability can be minimized with antiepileptic medications.
- Cautious monitoring to distinguish from TIAs.
- Cognitive Impairment
- Cognitive rehabilitation.
- Supportive treatments for memory and executive function.
- Seizures
- Treated with standard anti-seizure drugs.
Surgical/Interventional Options
- Limited; craniotomy can be necessary for life-threatening lobar hemorrhage.
Prognosis
- CNS involvement greatly exacerbates quality of life and survival.
- Microbleeds and TFNEs tend to precede massive hemorrhage.
- Cognitive decline evolves gradually and may outstrip systemic management.
Multidisciplinary Care Approach
ATTRv amyloidosis patients with CNS complications need synchronized care from:
- Neurologists – for cognitive, seizure, and stroke management.
- Geneticists – for family guidance and analysis of mutation.
- Hematologists/amyloidosis specialists – to maximize systemic therapy.
- Neuropsychologists – for cognitive rehabilitation.
- Support groups – to cope with progressive disability.
Future Directions in Research
- Therapies that cross the blood–brain barrier are developed.
- Intrathecally administered gene silencing to specifically target CNS TTR production.
- Enhanced neuroimaging biomarkers for the identification in early stages.
- Clinical trials targeting CNS outcomes in ATTRv.
Conclusion
CNS engagement in hereditary ATTRv amyloidosis is a critical but underappreciated complication. Leptomeningeal amyloidosis causes cerebral microbleeds, lobar hemorrhages, fleeting focal neurological syndromes, seizures, and worsening cognitive impairment.
Although systemic treatments for ATTRv have evolved considerably, their poor CNS penetration is a significant therapeutic problem. Present management relies on symptomatic control, hemorrhagic complications prevention, and supportive treatment.
Prompt identification of CNS symptoms in patients with established ATTRv—and proactive genetic screening in susceptible families—remains important. With ongoing research, therapies aimed at CNS amyloid deposits in the future promise improved outcomes.

