Table of Contents
Common symptoms of UTIs in AL Amyloidosis patients
AL amyloidosis is a rare systemic disorder characterized by the abnormal proliferation of plasma cells producing monoclonal light chains (either kappa or lambda). These light chains misfold and deposit as amyloid fibrils in various tissues and organs, leading to progressive organ dysfunction. Common Given the kidneys are frequently involved in AL amyloidosis—often manifesting as nephrotic syndrome, proteinuria, and progressive renal failure—patients are at increased risk for urinary complications, including urinary tract infections (UTIs).UTI symptoms in AL Amyloidosis patients
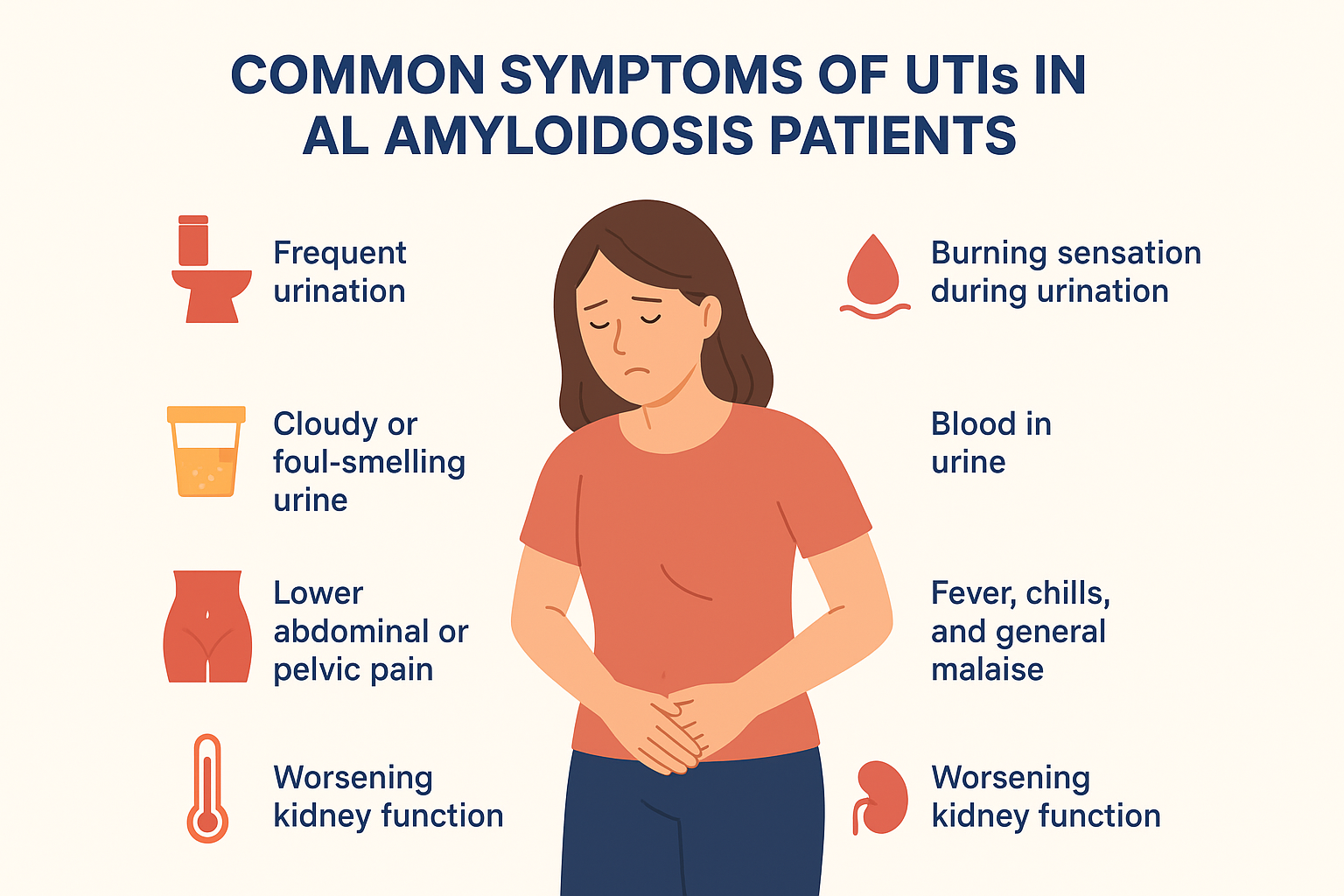
Amyloid deposits in the renal parenchyma and urinary tract structures can predispose to infections, urinary stasis, and other urinary symptoms.In patients with AL amyloidosis, the common symptoms of urinary tract infections (UTIs) often overlap with those seen in the general population but may present with added complexity due to underlying organ involvement. Typical signs include frequent urination, an urgent need to urinate, burning or pain during urination, and cloudy or foul-smelling urine. Some patients may also notice blood in the urine (hematuria) or experience lower abdominal or pelvic discomfort. In advanced cases, systemic symptoms like fever, chills, fatigue, and generalized weakness may develop, signaling the spread of infection. However, AL amyloidosis can mask or alter these symptoms because of neuropathy, bladder dysfunction, or renal involvement, making UTIs harder to recognize and sometimes leading to delayed diagnosis.
Pathophysiology of UTIs in AL Amyloidosis
AL (amyloid light-chain) amyloidosis is a systemic disorder characterized by the deposition of monoclonal immunoglobulin light-chain amyloid fibrils in multiple organs. The disease results from a clonal proliferation of plasma cells that produce excess light chains, which misfold and aggregate into amyloid fibrils. These deposits interfere with the normal structure and function of affected tissues, leading to progressive organ dysfunction .The kidneys are most commonly involved, often manifesting as proteinuria, nephrotic syndrome, and progressive renal failure.
The involvement of the urinary tract, although less frequent, significantly predisposes patients to urinary tract infections (UTIs). The pathophysiology of UTIs in AL amyloidosis is complex and multifaceted, involving structural, functional, and immunological factors This comprehensive analysis explores the mechanisms by which AL amyloidosis predisposes to UTIs, including amyloid deposition effects on urinary tract integrity, alterations in immune responses, urinary stasis, and secondary factors. Fever, chills, and general malaise – may indicate progression to upper UTI.
Common Symptoms of UTIs in AL Amyloidosis Patients
Urinary tract infections (UTIs) are among the most common bacterial infections affecting the urinary system, including the kidneys, ureters, bladder, and urethra. In the general population, typical symptoms include dysuria, urgency, frequency, and suprapubic discomfort. However, in patients with AL amyloidosis, the presentation can be atypical or masked due to the disease’s systemic effects, organ infiltration, immunosuppression, and comorbidities.AL amyloidosis, characterized by the deposition of misfolded immunoglobulin light chains as amyloid fibrils, primarily affects organs like the kidneys, heart, liver, and nervous system. When the urinary system is involved—either directly through amyloid infiltration or indirectly via secondary effects—the clinical manifestations of UTIs can be altered or complicated .This document explores the common symptoms of UTIs in AL amyloidosis patients, emphasizing typical and atypical presentations, pathophysiological underpinnings, and clinical considerations.
While UTIs in the general population usually present with well-recognized symptoms—such as dysuria, urgency, frequency, suprapubic pain, and occasionally hematuria—patients with AL amyloidosis may present with atypical, subtle, or overlapping symptoms, complicating timely diagnosis and management. Understanding the common symptoms of UTIs in AL amyloidosis patients is therefore essential for clinicians, caregivers, and patients themselves, as early recognition may significantly improve outcomes and prevent complications such as sepsis, worsening kidney damage, or progressive amyloid-related organ dysfunction. This article explores the clinical symptomatology of UTIs in AL amyloidosis, the pathophysiological basis for these manifestations, and the ways in which amyloid deposition alters classical urinary tract infection presentations.Dysuria: Painful or Burning Urination
Dysuria: Painful or Burning Urination
One of the most common and hallmark symptoms of UTIs in both the general population and AL amyloidosis patients is dysuria, or painful urination. The sensation is often described as a burning or stinging feeling during micturition. Bladder mucosal fragility due to amyloid infiltration, making the urothelium more vulnerable to bacterial adherence. Neuropathy, which may alter the pain threshold or change how patients perceive discomfort. Some patients report heightened burning sensations, while others describe dull, vague discomfort.Secondary complications such as candiduria (fungal infection), which is more common due to immunosuppressive therapies used in managing amyloidosis. Clinicians should recognize dysuria in amyloidosis patients as a red flag symptom, especially when associated with systemic complaints such as fatigue or worsening renal function
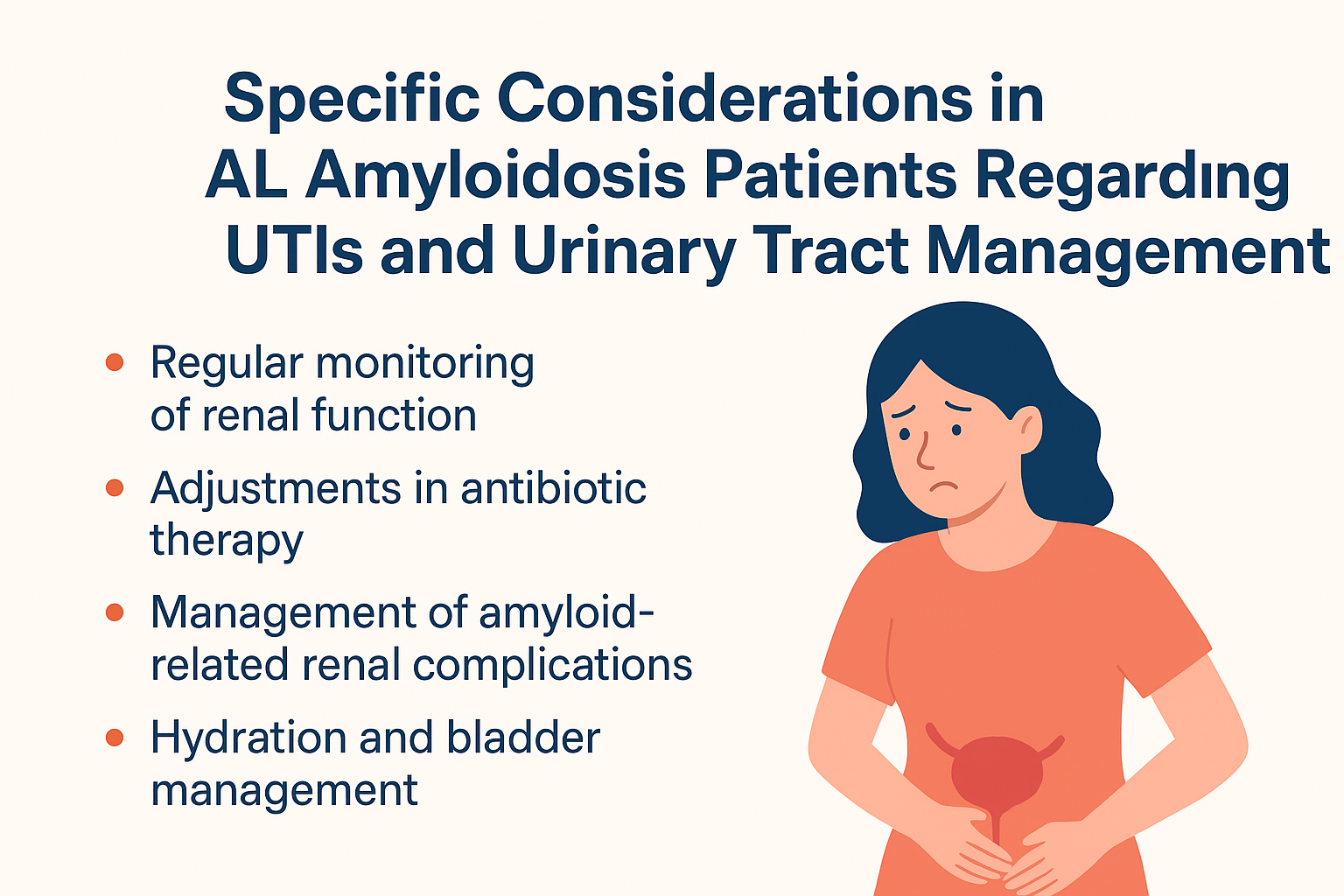
Specific Considerations in AL Amyloidosis Patients Regarding UTIs and Urinary Tract Management
AL (amyloid light-chain) amyloidosis is a complex systemic disorder characterized by the deposition of monoclonal immunoglobulin light chains as amyloid fibrils in multiple organs. Its multisystem involvement, organ-specific manifestations, and associated immunological and structural abnormalities pose unique challenges in managing urinary tract infections (UTIs).Patients with AL amyloidosis often present with atypical, subtle, or masked symptoms, owing to nerve infiltration, organ dysfunction, and immune suppression. These factors necessitate tailored clinical approaches, vigilant monitoring, and multidisciplinary strategies .This discussion explores the specific considerations in diagnosing, preventing, and managing UTIs in AL amyloidosis patients, emphasizing the importance of understanding disease pathology, comorbidities, and treatment implications.
Pathophysiological Basis of UTIs in AL Amyloidosis Patients
The pathophysiology of UTIs in patients with AL amyloidosis is multifaceted. Amyloid fibrils deposit in multiple organs, including the kidneys and urinary tract, leading to functional abnormalities that predispose to infection. Renal amyloid infiltration can impair glomerular filtration, alter tubular function, and compromise urinary concentration capacity. Moreover, autonomic neuropathy resulting from amyloid deposition in the peripheral nerves can cause neurogenic bladder dysfunction, incomplete emptying, and urinary stasis, which create an ideal environment for bacterial colonization.
Additionally, hypoimmunoglobulinemia, a common feature in amyloidosis patients due to plasma cell dyscrasia, weakens the immune system’s ability to fight infections. The impaired host defense makes these individuals more susceptible to recurrent and complicated UTIs. In many cases, patients are also undergoing treatment regimens such as chemotherapy, corticosteroids, or immunomodulatory agents, which further suppress immunity. This interplay of impaired immunity, organ dysfunction, and altered host defense represents the foundation for recurrent urinary tract infections in AL amyloidosis patients.Symptom Presentation in Amyloidosis Patients
The presentation of UTIs in AL amyloidosis patients may differ significantly from the general population. Classic symptoms such as dysuria, frequency, urgency, and suprapubic discomfort may still occur, but they can often be overshadowed by systemic symptoms related to amyloidosis or masked by neuropathy.Patients with autonomic dysfunction may not perceive bladder fullness or pain, leading to atypical presentations such as unexplained fever, fatigue, or worsening edema due to renal decline. In advanced cases, sepsis or acute kidney injury may be the first sign of an underlying urinary tract infection. Moreover, due to baseline proteinuria and hematuria associated with renal amyloidosis, it can be challenging to distinguish infection-related urinary abnormalities from disease-related findings.This atypical and often subtle presentation necessitates heightened clinical vigilance and proactive diagnostic screening in amyloidosis patients with even mild suspicion of infection.
Other Contributing Factors to UTI Pathogenesis
Urinary tract infections (UTIs) are among the most common bacterial infections affecting humans worldwide. While the primary etiological agent in most cases is Escherichia coli (especially uropathogenic E. coli or UPEC), it is now well established that the pathogenesis of UTIs is not determined solely by the infecting organism. Multiple other contributing factors—including host-related, behavioral, anatomical, hormonal, iatrogenic, microbial, environmental, and socioeconomic influences—play a crucial role in determining susceptibility, recurrence, and severity of infection. Understanding these factors is critical, not only for clinical diagnosis and treatment but also for designing preventive strategies in at-risk populations.
This article explores, in detail, the other contributing factors to UTI pathogenesis beyond microbial infection alone. Another critical host factor is genetic susceptibility. Research has demonstrated that certain individuals have genetic variations that make them more prone to UTIs, including polymorphisms in innate immune system receptors such as Toll-like receptors (TLRs). These receptors play a role in recognizing bacterial components like lipopolysaccharides (LPS) and triggering immune responses.

