Congestive Hepatopathy in AL Amyloidosis:
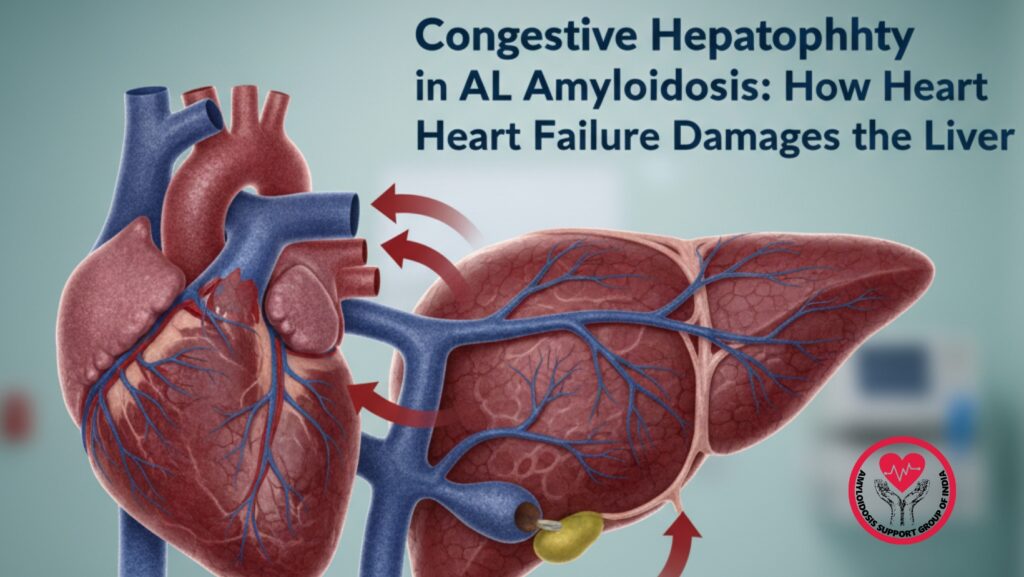
Table of Contents
Introduction
AL amyloidosis is a complex disease where misfolded light-chain proteins build up in various organs, progressively damaging their function. Although the kidneys, heart, and nervous system are the most commonly affected, one important but lesser-known complication is congestive hepatopathy, a type of liver dysfunction caused by chronic blood congestion in the liver.
In AL amyloidosis, congestive hepatopathy occurs when right-sided heart failure hinders the effective return of blood from the venous system to the heart. As pressure increases in the inferior vena cava and hepatic veins, the liver becomes engorged with blood, inflamed, and eventually damaged.
This article examines the mechanisms, symptoms, diagnostics, and implications of congestive hepatopathy in AL amyloidosis. It aims to help patients, families, and healthcare professionals understand how heart failure affects the liver and why early detection is crucial for better outcomes.
1. Understanding AL Amyloidosis and Its Multi-Organ Effects
1.1 What is AL Amyloidosis?
AL (light-chain) amyloidosis is a plasma cell disorder in which abnormal immunoglobulin light chains misfold and clump together into beta-pleated sheets. These amyloid fibrils deposit in tissues and gradually interfere with organ structure and function.
Common places for deposition include:
- Heart
- Kidneys
- Liver
- Gastrointestinal tract
- Peripheral nerves
- Autonomic nerves
- Soft tissues
The disease progresses and can be fatal if not caught early.
1.2 How AL Amyloidosis Affects the Cardiovascular System
The heart is one of the most affected organs in AL amyloidosis. Amyloid deposits stiffen the ventricular walls, causing restrictive cardiomyopathy. This leads to:
- Impaired filling
- Reduced stroke volume
- Low cardiac output
- High central venous pressure
- Heart failure, especially right-sided
Right heart failure connects cardiac amyloidosis to congestive hepatopathy.
2. What Is Congestive Hepatopathy?
2.1 Definition
Congestive hepatopathy refers to liver dysfunction due to long-term increased central venous pressure, usually caused by right-sided heart failure.
2.2 Why It Occurs
Blood from the liver normally drains into the inferior vena cava through the hepatic veins. When right-sided pressures rise, blood cannot leave the liver effectively, causing:
- Hepatic venous congestion
- Dilatation of sinusoids
- Reduced oxygen diffusion
- Cellular injury
- Fibrosis (over time)
In advanced stages, congestive hepatopathy may lead to cardiac cirrhosis.
3. The Connection Between AL Amyloidosis and Congestive Hepatopathy
3.1 How Amyloid Infiltration Leads to Heart Failure
Amyloid proteins build up in the ventricular walls, making the heart stiff and less compliant. The right ventricle, which is thinner and more pressure-sensitive than the left ventricle, becomes especially at risk.
3.2 The Cascade That Leads to Liver Damage
As the right ventricle fails:
- Blood cannot move forward into the lungs.
- Pressure builds in the right atrium.
- Backward pressure travels into the venous system.
- This pressure rises in the IVC and hepatic veins.
- The liver becomes swollen and deprived of oxygen.
This vascular bottleneck illustrates how cardiac amyloidosis directly leads to liver disease.
3.3 Why the Liver Is Vulnerable
The liver receives blood from two main sources:
- Portal vein (70%)
- Hepatic artery (30%)
However, hepatic veins only drain blood toward the heart. When this flow is blocked, congestion follows.
4. Early Signs and Symptoms of Congestive Hepatopathy
4.1 Early or Mild Symptoms
Early congestive hepatopathy may not show obvious signs, but subtle indications include:
- Fatigue
- Malaise
- Loss of appetite
- Mild discomfort in the right upper abdomen
- Slight liver enlargement
Many patients do not recognize symptoms until congestion becomes severe.
4.2 Progressive Symptoms
As venous pressure increases:
- Right upper quadrant pain
- Feeling of abdominal fullness
- Abdominal bloating
- Nausea
- Early satiety
- Visible JVD (jugular vein distension)
- Swelling in legs and feet
4.3 Advanced Symptoms
Advanced congestive hepatopathy can result in:
- Jaundice
- Ascites
- Elevated INR (due to reduced clotting factor production)
- Hepatic encephalopathy (rare, but possible)
These symptoms can mimic those of primary liver diseases, but the cause is rooted in heart failure.
5. What Happens Inside the Liver During Congestion?
5.1 Sinusoidal Dilation
High venous pressure causes the hepatic sinusoids to dilate. This makes it harder for liver cells to receive oxygen.
5.2 Hepatocyte Hypoxia
As congestion worsens, hepatocytes near central veins get less oxygen, resulting in “centrilobular necrosis.”
5.3 Fibrosis and Long-Term Damage
Chronic congestive hepatopathy leads to:
- Collagen buildup
- Fibrotic bands
- A “nutmeg liver” appearance
- Eventually, cardiac cirrhosis
Amyloid deposits can also occur in the liver, but they usually play a smaller role in dysfunction compared to congestion.
6. Diagnosis of Congestive Hepatopathy in AL Amyloidosis
6.1 Clinical Examination
Key findings include:
- Increased jugular venous pressure
- Hepatomegaly
- Tenderness in the liver
- Swelling in the limbs
- Ascites
6.2 Laboratory Tests
Blood tests may reveal:
- Mildly elevated bilirubin
- Increased alkaline phosphatase
- Mild transaminitis
- Low albumin levels
- Elevated INR (in serious cases)
6.3 Imaging Studies
Ultrasound
Shows:
- Enlarged liver
- Dilated hepatic veins and IVC
- Decreased respiratory collapse of IVC
CT or MRI
Shows:
- Nutmeg liver pattern
- Congestion around hepatic veins
Echocardiography
Crucial for identifying the cause:
- Reduced ventricular compliance
- Thickened walls
- Diastolic dysfunction
- Enlarged right atrium
- Increased right-sided pressures
6.4 Liver Biopsy
Rarely needed, but if performed, may show:
- Sinusoidal dilation
- Centrilobular fibrosis
- Amyloid deposits
7. Management and Treatment Strategies
7.1 Treating the Root Cause: Cardiac Amyloidosis
Chemotherapy
Used to suppress plasma cells producing light chains:
- Bortezomib-based regimens (e.g., CyBorD)
- Daratumumab combinations
- Autologous stem cell transplantation (for selected patients)
Supportive Treatment for Heart Failure
- Cautious use of diuretics
- Low salt intake
- Management of arrhythmias
- Avoidance of beta blockers and calcium channel blockers (often poorly tolerated)
7.2 Managing Liver Congestion
Lifestyle and Supportive Measures
- Low-salt diet
- Avoiding alcohol
- Regular monitoring
Fluid and Diuretic Management
Helps alleviate pressure on the venous system, reducing liver congestion.
Treating Complications
Ascites may require diuretics or paracentesis. Coagulopathy should be closely monitored.
7.3 Why Liver-Specific Treatments Alone Don’t Work
The liver damage does not stem from liver disease itself but from heart failure. Treating the heart is essential.
8. Prognosis and Long-Term Outcomes
8.1 Impact of Cardiac Amyloidosis on Survival
Cardiac involvement is the strongest predictor of outcomes in AL amyloidosis.
8.2 Reversibility of Congestive Hepatopathy
The liver is resilient. If right-sided pressures decrease:
- Congestion can improve
- Liver enzymes can return to normal
- Hepatic fibrosis may stabilize
However, without treatment, progressive damage can lead to cirrhosis.
9. Patient Care Perspective: Recognizing Symptoms Early
Patients often miss early signs of liver congestion because they resemble regular symptoms of heart failure. It is crucial to seek evaluation for symptoms like:
- Bulging neck veins
- Swelling in the legs
- Fullness in the right abdomen
- Rapid weight gain
- Increasing fatigue
Early detection greatly improves outcomes.
10. Conclusion
Congestive hepatopathy in AL amyloidosis is a serious but often overlooked complication. It happens when the failing right heart struggles to manage venous return, causing pressure to build that directly affects the liver. Over time, this pressure damages liver cells, reduces liver function, and can advance to fibrosis or cardiac cirrhosis.
Grasping the link between cardiac amyloidosis and liver congestion is key for early diagnosis, effective treatment, and better survival rates. The focus should be on treating the root cause — the amyloid-related heart failure — while monitoring and managing liver symptoms.
With early intervention, modern chemotherapy, and supportive care, many patients can see significant improvement and avoid long-term liver damage.

