Eight Clinical Domains of Supportive Care in Systemic Amyloidosis: ISA Guidelines Explained
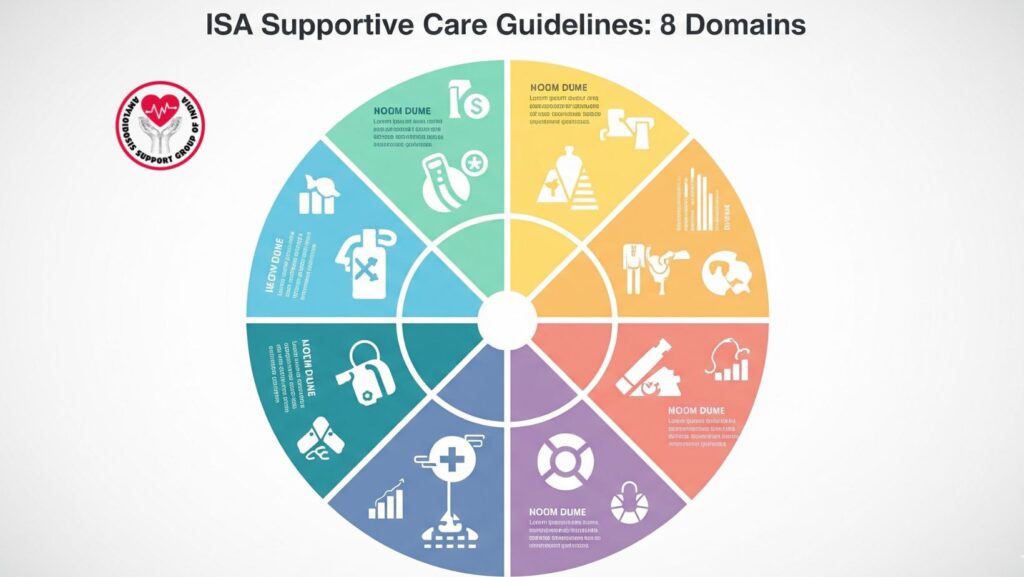
Table of Contents
1. Introduction
Systemic amyloidosis is a rare and multifaceted disorder where misfolded proteins accumulate in organs and cause progressive dysfunction. Although type-specific therapies (e.g., chemotherapy in AL amyloidosis or tafamidis in ATTR amyloidosis) address the root cause, they may have a lag time before clinical improvement.
Throughout this time, patients experience severe difficulties — fluid overload, heart failure, renal impairment, neuropathy, gastrointestinal disturbances, and nutritional deterioration. To fill this gap, the International Society of Amyloidosis (ISA) has formulated guidelines that place supportive care at the forefront of amyloidosis management.
These guidelines are organized into eight clinical domains:
- Cardiology
- Nephrology
- Peripheral neuropathy
- Central nervous system (CNS) involvement
- Autonomic neuropathy
- Gastroenterology
- Coagulopathy and bleeding
- Nutrition and hematology
2. The Importance of Supportive Care in Amyloidosis
- Bridges the gap between diagnosis and effective disease-modifying therapy.
- Improves quality of life by controlling symptoms like edema, neuropathy, or diarrhea.
- Supports organ function, preventing further deterioration.
- Improve survival, enabling patients to survive systemic therapies.
- Multidisciplinary practice, with the participation of cardiologists, nephrologists, hepatologists, neurologists, and dietitians.
3. The Eight Clinical Domains of Supportive Care
3.1 Cardiology: Managing Cardiac Involvement
The heart is commonly involved, especially in AL and ATTR amyloidosis. Amyloid deposition leads to restrictive cardiomyopathy, heart failure, and arrhythmias.
Key supportive strategies include:
- Diuretics (loop diuretics, spironolactone) to alleviate fluid overload and edema.
- Titration of fluid balance to prevent hypotension or aggravation of renal failure.
- Low-sodium diet to manage ascites and swelling.
- Pacemakers or defibrillators in the case of conduction defects or ventricular arrhythmias.
- Careful use/avoidance of certain medications (e.g., beta-blockers, ACE inhibitors, calcium channel blockers), as they can aggravate prognosis in amyloid cardiomyopathy.
3.2 Nephrology: Preserving Kidney Function
Renal involvement is characterized by proteinuria, nephrotic syndrome, and chronic kidney disease.
Supportive measures are:
- ACE inhibitors/ARBs to decrease proteinuria and retard renal damage.
- Diuretics for control of edema.
- Low-salt, moderate-protein diet to avoid fluid retention and strain.
- Dialysis for individuals with end-stage renal failure.
- Delicate medication adjustments to prevent nephrotoxic drugs.
Renal supportive care stabilizes patients and renders them candidate for renal transplantation in some cases.
3.3 Peripheral Neuropathy: Pain and Function
Amyloid deposits cause injury to peripheral nerves, resulting in sensory loss, pain, weakness, and mobility impairment.
Supportive measures are:
- Neuropathic pain management with gabapentin, pregabalin, duloxetine, or tricyclic antidepressants.
- Physical therapy for muscle strength and balance.
- Assistive devices such as braces, canes, or orthotics.
- Occupational therapy for adaptations in daily activity.
3.4 Central Nervous System (CNS) Involvement
CNS involvement is not frequent but occurs in some hereditary amyloidoses (e.g., variants of ATTR). Patients can experience stroke, cognitive impairment, or seizures.
Supportive strategies include:
- Regular neurological monitoring with imaging and cognitive assessments.
- Antiepileptic drugs for seizures.
- Cognitive support therapies for memory and functional challenges.
- Rehabilitation programs for stroke recovery.
3.5 Autonomic Neuropathy: Stabilizing Vital Functions
Autonomic dysfunction can cause orthostatic hypotension, bowel irregularities, urinary problems, and erectile dysfunction.
Supportive strategies include:
- Midodrine or fludrocortisone for orthostatic hypotension.
- Salt supplementation and compression stockings for circulatory support.
- Laxatives or antidiarrheal for bowel abnormalities.
- Bladder management techniques such as catheterization or timed voiding.
3.6 Gastroenterology: GI and Nutritional Support
GI amyloidosis can lead to diarrhea, constipation, GI bleeding, and malabsorption.
Supportive interventions are:
- Nutritional counseling to support body weight and energy maintenance.
- Prokinetic agents or antidiarrheals (loperamide) for regulation of bowel.
- Vitamin and iron supplementation for malabsorption.
- Parenteral nutrition in serious weight loss.
3.7 Coagulopathy and Bleeding
Amyloidosis can impair coagulation due to amyloid deposition in vessels and liver failure.
Supportive measures include:
- Monitoring clotting function on a regular basis.
- Plasma exchange or factor replacement in cases of severe bleeding episodes.
- Anticoagulant use carefully due to bleeding risk.
- Close hematology specialist coordination.
3.8 Nutrition and Hematology
Malnutrition and anemia are common due to chronic disease, GI disease, and renal disease.
Supportive measures include:
- High-protein, high-calorie diets to sustain strength.
- Supplementation with vitamin D, calcium, and iron.
- Erythropoiesis-stimulating agents for anemia secondary to chronic kidney disease.
- Routine weight and nutritional monitoring.
4. Multidisciplinary Approach
ISA guidelines also highlight that supportive care should be provided through a team effort. Coordination between cardiologists, nephrologists, neurologists, hepatologists, dietitians, and palliative care professionals ensures patients get detailed and individualized care.
5. Conclusion
Supportive care in systemic amyloidosis is not adjunctive — it is a pillar of management. Attending to eight key domains (cardiology, nephrology, peripheral neuropathy, CNS, autonomic neuropathy, gastroenterology, coagulopathy, and nutrition/hematology), the clinician can substantially enhance survival, quality of life, and treatment outcome.
The ISA supportive care guidelines give a blueprint for global management, reminding clinicians that successful care involves both disease-targeting therapies and strong supportive interventions.

