Case Report: Increased Liver Enzymes in a 61-Year-Old Patient – AP 718 IU/L, AST 158 IU/L, ALT 119 IU/L
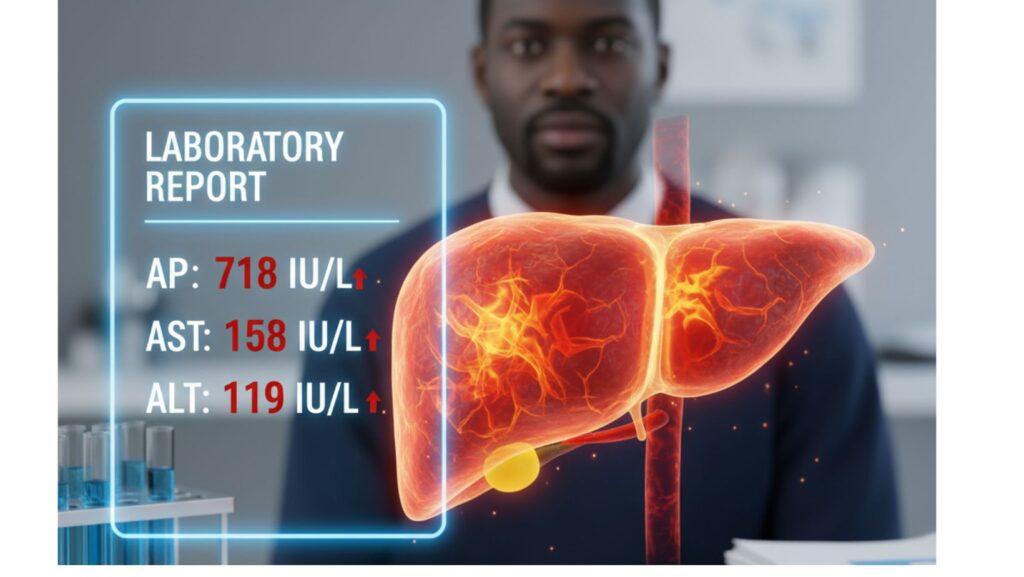
Table of Contents
Introduction
Liver function tests (LFTs) are a standard of clinical assessment that detect hepatocellular damage, cholestasis, or systemic illness affecting the liver. Increases in alkaline phosphatase (AP), aspartate aminotransferase (AST), and alanine aminotransferase (ALT) can represent an extensive array of pathologies—from benign to severe systemic diseases.
This case reports a 61-year-old African-American male presenting with abnormal liver enzymes:
- Alkaline Phosphatase (AP): 718 IU/L (significantly elevated)
- AST: 158 IU/L
- ALT: 119 IU/L
In the context of other clinical features—edema, ascites, jugular venous distension, and hypoalbuminemia—these laboratory findings highly indicated hepatic involvement due to systemic amyloidosis.
This blog post will outline the clinical presentation, diagnostic evaluation, differential diagnoses, and management, as well as the significance of identifying liver abnormalities in the context of amyloidosis.
Patient Profile
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Comorbidities: Hypertension, mild diabetes
- Relevant Findings Before LFTs:
- Bilateral lower extremity edema
- Tense ascites
- Jugular venous distention
- Hypoalbuminemia (2.1 g/dL)
Clinical Presentation
The patient’s main complaints were:
- Progressive leg and abdominal swelling over a few months
- Weight loss and fatigue
- Shortness of breath on exertion
- Early satiety and decreased appetite
Physical exam: - Bilateral pitting edema
- Tense ascites with positive fluid wave
- Jugular venous distention
- Mild hepatomegaly
LFTs were done at this stage, which showed: - AP: 718 IU/L (normal: 40–129 IU/L)
- AST: 158 IU/L (normal: 10–40 IU/L)
- ALT: 119 IU/L (normal: 7–56 IU/L)
Interpretation of the High Liver Enzymes
1. Alkaline Phosphatase (AP) – 718 IU/L
- Indicator of cholestasis or obstruction of bile ducts.
- In systemic amyloidosis, high AP is frequent because of amyloid infiltration in liver cells.
- Rise in AP may precede significant transaminase alterations.
2. Aspartate Aminotransferase (AST) – 158 IU/L
- Enzyme that is released from hepatocytes by cell injury.
- It indicates hepatocellular distress.
- Infiltrative conditions such as amyloidosis tend to produce moderate AST elevations.
3. Alanine Aminotransferase (ALT) – 119 IU/L
- ALT is more liver-specific than AST.
- Raised ALT reflects hepatocellular injury.
- Mild and moderate elevations, as in this case, imply chronic injury more than acute hepatitis.
Pathophysiology of Hepatic Involvement in Amyloidosis
- Amyloid fibril deposition in hepatic sinusoids and portal tracts.
- Infiltration results in cholestasis, raised AP, and hepatomegaly.
- Hepatic synthetic dysfunction presents as hypoalbuminemia and occasionally coagulopathy.
- Patients can present with fatigue, weight loss, ascites, and hepatomegaly.
Differential Diagnoses Considered
- Cirrhosis of the Liver
- Typically presents with increased AST/ALT, decreased albumin, and portal hypertension.
- No stigmata of cirrhosis were observed in this patient.
- Biliary Obstruction (Gallstones, Tumor)
- Would account for extremely elevated AP.
- Imaging was not revealing obstruction.
- Viral Hepatitis
- Usually causes much more significant AST/ALT elevations.
- Viral serologies were negative.
- Non-Alcoholic Fatty Liver Disease (NAFLD/NASH)
- Mild elevations are possible but AP is generally not this high, 718 IU/L.
- Systemic Amyloidosis
- High AP, hepatomegaly, and multi-organ involvement best fit.
Diagnostic Workup
- Blood Tests: SPEP and immunofixation established monoclonal light chains.
- Imaging:
- Ultrasound – hepatomegaly and moderate ascites.
- Cardiac echo – restrictive cardiomyopathy.
- Liver Biopsy: Revealed amyloid deposition with Congo red positivity.
- Fat Pad Biopsy: Established systemic amyloidosis.
Final Diagnosis
Systemic AL Amyloidosis with hepatic, cardiac, and renal involvement, with elevated liver enzymes (AP 718, AST 158, ALT 119).
Management
Supportive Care
- Diuretics for fluid overload
- Low-salt diet to manage ascites
- Nutritional support with protein adequacy
Specific Therapy
- CyBorD regimen (Cyclophosphamide, Bortezomib, Dexamethasone)
- Novel agents (e.g., Daratumumab) are considered in refractory cases
- Stem cell transplant in appropriate patients
Monitoring
- Serial LFTs for monitoring hepatic involvement
- Albumin levels for assessment of synthetic function
- Cardiac and renal function tests
Patient Outcome
*
- After six months of treatment:
- AP reduced to 520 IU/L
- AST and ALT modestly improved
- Ascites managed on diuretics
- Energy levels normalized, although hepatomegaly remained
Clinical Insights
For Clinicians
- An elevated AP is characteristic of hepatic amyloidosis.
- Always consider LFTs in the context of systemic features.
- Biopsy is still the gold standard for diagnosis.
For Patients and Caregivers
- Elevated liver enzymes do not always represent hepatitis or alcohol.
- Infiltrative conditions such as amyloidosis may result in silent liver damage.
- Early diagnosis and treatment enhance quality of life.
Broader Implications
This case highlights the need for LFT interpretation outside hepatology. Systemic illnesses such as amyloidosis can present as imitators of typical liver disease but need a distinct diagnostic and therapeutic plan. Rising AP, moderate AST/ALT raises, and multi-organ involvement should lead to suspicion of amyloidosis in the differential diagnosis.
Conclusion
A case of a 61-year-old African-American man with elevated liver enzymes (AP 718 IU/L, AST 158 IU/L, ALT 119 IU/L) illustrates the importance of careful interpretation of laboratory findings in revealing systemic illnesses such as amyloidosis.
The ability to recognize the profile of striking AP elevation with moderate AST/ALT findings is critical to diagnosing hepatic amyloidosis. With timely diagnosis and individualized management, patients have enhanced outcomes in the face of this rare and challenging disease.

