Case Report: Bililateral Lower Extremity Edema, Ascites, and Jugular Venous Distention – Important Physical Exam Findings
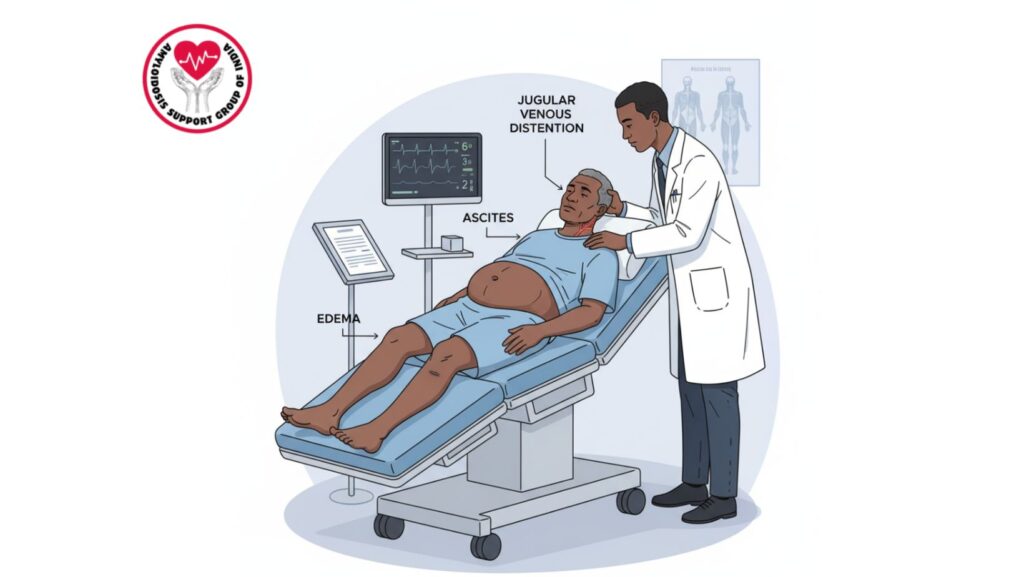
Table of Contents
Introduction
Physical exam continues to be the foundation of clinical medicine. Although new diagnostic technologies have revolutionized healthcare, the bedside examination often yields the initial key clues that lead clinicians to a diagnosis.
This case report introduces a 61-year-old African-American male who had three classic physical findings:
- Bilateral lower extremity edema
- Tense ascites
- Jugular venous distention (JVD)
These observations strongly suggested a systemic pathology with multi-organ involvement, subsequently proven to be amyloidosis. This blog post will therefore discuss the case in detail, from presentation to diagnosis and management, presenting both clinical insights for professionals and awareness for patients and carers.
Why These Physical Findings Matter
1. Bilateral Lower Extremity Edema
- Definition: Bilateral swelling of the legs due to fluid retention.
- Common Causes: Heart failure, kidney disease, liver disease, venous insufficiency.
- In Amyloidosis: Usually secondary to cardiac dysfunction or nephrotic-range proteinuria.
2. Tense Ascites
- Definition: Peritoneal cavity accumulation of fluid resulting in abdominal distension.
- Common Causes: Cirrhosis, malignancy, heart failure, hypoalbuminemia.
- In Amyloidosis: Can occur due to hepatic infiltration or right-sided heart failure.
3. Jugular Venous Distention (JVD)
- Definition: Visible jugular vein distension that is an indicator of increased central venous pressure.
- Common Causes: Right-sided heart failure, pericardial disease, restrictive cardiomyopathy.
- In Amyloidosis: Important finding of restrictive cardiomyopathy caused by amyloid deposition.
Patient Profile
The patient was:
- Age: 61 years
- Ethnicity: African-American
- Gender: Male
- Comorbidities: Hypertension, mild diabetes
- Chief Complaint: Swelling of the legs, abdominal distension, and shortness of breath over a few months
Clinical Presentation
The patient had:
- Progressive leg swelling for > 2 months
- Abdominal distension with pain and early satiety
- Shortness of breath on exertion
- Fatigue and weight loss
- Peripheral neuropathy symptoms (numbness, tingling in feet)
On examination: - Bilateral pitting edema to knees
- Tense ascites with fluid thrill
- Jugular venous distention palpable at 45° angle
- Mild hepatomegaly
- Clear lungs, but decreased exercise tolerance
These three findings — edema, ascites, and JVD — were very suggestive of systemic congestion due to cardiac dysfunction.
Diagnostic Evaluation
Laboratory Investigations
- CBC: Mild anemia
- Renal Function: Slightly elevated creatinine
- Liver Function Tests: Low albumin, mild elevation of enzymes
- Urinalysis: Proteinuria revealed
- Serum Protein Electrophoresis (SPEP): Monoclonal spike
- Immunofixation: Confirmation of light chains
Imaging Studies
- Echocardiography: Thickening of ventricular wall, diastolic dysfunction
- Cardiac MRI: Confirmation of restrictive cardiomyopathy due to amyloid infiltration
- Ultrasound Abdomen: Moderate ascites, hepatomegaly
Biopsy
- Fat Pad Biopsy: Congo red positive (apple-green birefringence)
- Subtyping: AL Amyloidosis confirmed
Differential Diagnosis Considered
- Cirrhosis of the Liver – ruled out on the basis of intact clotting factors and absence of stigmata of liver disease.
- Nephrotic Syndrome – found but secondary to amyloid deposition.
- Right-Sided Heart Failure – established but secondary to amyloidosis and not primary cardiac disease.
- Peritoneal Malignancy – ruled out by imaging and cytology.
Final Diagnosis
Systemic AL Amyloidosis with cardiac, renal, and hepatic involvement, with presenting symptoms of bilateral lower extremity edema, tense ascites, and jugular venous distension.
Treatment Plan
1. Supportive Therapy
- Diuretics for management of edema and ascites
- Paracentesis for symptomatic control of ascites
- Restriction of salt in diet
- Compression stockings for leg swelling
2. Disease-Specific Treatment
- Bortezomib + Cyclophosphamide + Dexamethasone (CyBorD regimen)
- Autologous Stem Cell Transplant: Deliberated but postponed owing to cardiac complications
3. Monitoring
- Renal and liver function tests on a monthly basis
- Routine cardiac imaging
- Hematologic follow-up on light chain levels
Patient Outcome
- Beyond 6 months, edema and ascites resolved with treatment.
- Jugular venous pressure reduced but did not return to normal.
- Cardiac symptoms stabilized.
- Partial hematologic remission achieved.
- Quality of life significantly improved with supportive therapy.
Clinical Insights
For Clinicians
- Physical exam findings remain invaluable. In this patient, three signs guided the diagnosis.
- Early biopsy is critical. Fat pad biopsy provided confirmation.
- Think systemic. When multiple organs are involved, consider amyloidosis.
- Team-based care works best. Coordination between hematology, cardiology, and hepatology improved management.
For Patients & Caregivers
- Do not ignore persistent swelling. It may indicate a systemic condition.
- Seek specialized centers. Rare diseases need expert evaluation.
- Lifestyle interventions (diet, fluid management, exercise) complement medical care.
- Support groups like Amyloidosis Support India offer emotional and practical advice.
Broader Implications
This case highlights the way time-honored bedside observations such as JVD, ascites, and edema are still compelling diagnostic tools. Even with the presence of MRI and high-tech laboratory tests, the stethoscope and examiner’s eye cannot be replaced.
In addition, it demonstrates the necessity to raise awareness of amyloidosis in India and globally. Earlier diagnosis might result in earlier treatment, fewer complications, and enhanced survival.
Conclusion
The presentation of a 61-year-old African-American man with bilateral lower extremity edema, tense ascites, and jugular venous distension emphasizes the value of meticulous physical examination in the diagnosis of systemic illnesses such as amyloidosis.
Through the incorporation of clinical skills, diagnostic tests, and multidisciplinary care, rare condition patients can have improved outcomes. This case serves as a reminder that the body often provides the first clues—clinicians just need to listen and observe.

