Laboratory Abnormalities in Liver Involvement of AL Amyloidosis – Understanding Mild LFT Elevations and Hypoalbuminemia
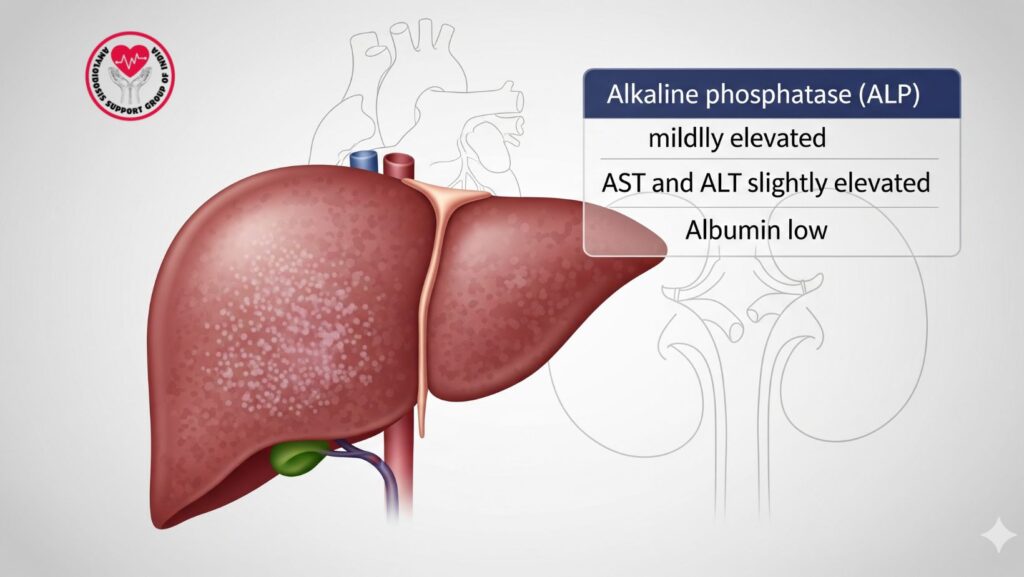
Table of Contents
Introduction
AL (primary) amyloidosis is a systemic illness wherein misfolded immunoglobulin light chains are deposited as amyloid fibrils in organs. Among these organs, the liver is frequently involved, yet clinical presentation tends to be mild. Laboratory abnormalities are usually the initial sign of involvement of the liver.
Appreciation of pattern and significance of abnormality in liver function tests (LFT)—specifically mild increases in alkaline phosphatase (ALP) and transaminases (AST, ALT) and hypoalbuminemia—is important for:
Early recognition of liver involvement
Risk stratification and prognosis
Therapeutic decision-making
Monitoring disease
This handbook reviews:
Overview of AL amyloidosis
Mechanisms of liver involvement
Typical laboratory findings
Interpretation of LFTs and clinical implications
Differential diagnosis of hepatic dysfunction in amyloidosis
- Diagnostic strategy and workup
- Management principles and monitoring
- Clinical pearls and case studies
- Research directions in the future
Epidemiology of Liver Involvement
- 60–90% of systemic AL amyloidosis patients have some extent of liver involvement.
- The majority of cases are clinically silent with minimal lab abnormalities.
- Symptomatic liver disease is infrequent but may present as:
- Hepatomegaly
- Mild jaundice
- Portal hypertension in advanced disease
- Male dominance and advanced age are typical in hepatic amyloidosis patients.
Pathophysiology of Hepatic Involvement
Mechanisms of Amyloid Deposition in the Liver
- Sinusoidal infiltration:
- Amyloid deposits in the space of Disse between sinusoids and hepatocytes
- Results in compression of hepatocytes and minor cholestasis
- Vascular involvement:
- Amyloid in hepatic arterioles and portal veins
- May lead to portal hypertension
- Impaired synthetic function:
- Progressive deposition can decrease albumin synthesis
- Transaminases may be mildly elevated but indicate hepatocellular stress and not necrosis
Common Laboratory Abnormalities
1. Alkaline Phosphatase (ALP)
- Usually mildly increased (1.5–3x upper limit of normal)
- Usually disproportionate from other LFTs
- Indicates cholestatic pattern due to amyloid deposition in bile canaliculi or sinusoids
2. Transaminases (AST and ALT)
- Normally mildly raised
- Rises seldom above 2–3x upper limit of normal
- Reflects hepatocellular stress instead of necrosis
- AST usually slightly above ALT
3. Albumin
- Low serum albumin is frequent
- Can be due to:
- Decreased hepatic production
- Urinary loss if coexistent nephrotic syndrome exists
- Hypoalbuminemia causes edema and ascites
4. Bilirubin
- Frequent or minimal elevation
- Prognostic value is uncertain, but study is worthwhile
- In liver, results are notoriously unreliable
- Significant hyperbilirubinemia uncommon but suggests advanced disease
5. Coagulation Parameters
- INR typically normal early
- Prolongation is found in advanced hepatic amyloidosis or multi-organ involvement
Clinical Significance of Lab Abnormalities
*
- Mild ALP elevation can be the earliest laboratory indication of liver involvement
- Low albumin can precede other clinical findings like ascites or edema
- AST/ALT elevations can distinguish amyloidosis from other liver conditions
- Lab trend monitoring is necessary for:
- Monitoring for progression
- Assessment of response to treatment
- Risk stratification
Differential Diagnosis
When assessing mild LFT abnormalities in AL amyloidosis, keep in mind:
- Non-amyloid etiologies:
- Viral hepatitis (HAV, HBV, HCV)
- Alcoholic liver disease
- Non-alcoholic fatty liver disease (NAFLD)
- Medication-related liver injury
- Chemotherapy or supportive therapy drugs may cause an elevation in transaminases
- Underlying systemic conditions
- Heart failure leading to congestive hepatopathy
- Renal illness leading to hypoalbuminemia
- Other infiltrative liver diseases
- Sarcoidosis
- Hemochromatosis
- Primary biliary cholangitis
Diagnostic Approach
Laboratory Evaluation
- Comprehensive LFT panel: ALP, AST, ALT, bilirubin, albumin, INR
- Renal function tests: Evaluate for concomitant nephrotic syndrome
- Serum protein electrophoresis and immunofixation: Identify monoclonal proteins
- Serum free light chain assay: Measure amyloidogenic light chains
Imaging Tests
- Ultrasound: Identify hepatomegaly, coarse echotexture
- CT/MRI: Evaluate liver size, infiltrative patterns, vascular flow
- Elastography: Optional for fibrosis evaluation
Biopsy of the Liver
- Gold standard for definitive diagnosis
- Congo red staining proves amyloid deposits
- Mass spectrometry detects AL type amyloid
Treatment Approaches
Disease-Modifying Therapy
- Chemotherapy (bortezomib, cyclophosphamide, dexamethasone): Decreases light chain production
- Stem cell transplantation: Reserved for carefully selected patients with maintained organ function
- Novel therapies: Investigational anti-amyloid monoclonal antibodies
Supportive Care
- Nutritional support: Reverse hypoalbuminemia
- Diuretics: Treat edema or ascites due to low albumin
- Monitoring: Frequent LFTs and cardiac/renal monitoring
Prognosis
- Mild lab abnormalities can be static for years
- Ascending to cholestatic liver failure is unusual but highly lethal
- Trends on lab are predictive of overall survival and multi-organ involvement
Case Studies
- Patient A: 61-year-old male, mild elevation of ALP (718 IU/L), albumin 2.1 g/dL, diagnosed on sigmoid biopsy. Developed severe hepatic involvement in months.
- Patient B: 58-year-old female, asymptomatic, mild AST/ALT elevation, albumin preserved. Prompt detection facilitated chemotherapy on time and stabilization of LFTs.
- Patient C: 65-year-old man, established AL amyloidosis complicated by cholestatic liver failure, ALP 1200 IU/L, albumin 1.8 g/dL. Supportive treatment started; survival ~3 months after jaundice onset.
Clinical Pearls
- Lab abnormalities that are mild should not be overlooked in systemic AL amyloidosis patients.
- ALP increase may be more dramatic than AST/ALT in hepatic amyloidosis.
- Monitoring for trends is more significant than absolute values.
- Early detection and treatment can slow progression and enhance outcomes.
- Multi-organ assessment is important due to common cardiac and renal involvement.
Future Directions
*
- Biomarker development: Increased sensitivity of markers for early hepatic amyloidosis
- Imaging advances: Quantitative MRI and PET scans for amyloid load
- Targeted therapies: Antibodies against fibrils and RNA-based treatments
- Personalized medicine: Treatment based on organ involvement and laboratory profile
- Longitudinal studies: Aligning laboratory trends with survival and response to therapy
Conclusion
Laboratory derangements—mildly elevated ALP and transaminases, low albumin—are the signature of hepatic involvement in AL amyloidosis. Identification of these patterns enables:
- Early detection of hepatic involvement
- Risk stratification for therapeutic selection
- Monitoring for disease progression and response to therapy
- Enhanced patient outcomes through prompt intervention
Clinicians must have a high index of suspicion in those with systemic AL amyloidosis and minimal hepatic lab changes to provide thorough, multidisciplinary treatment.

