Portal Hypertension as a Cause of Ascites
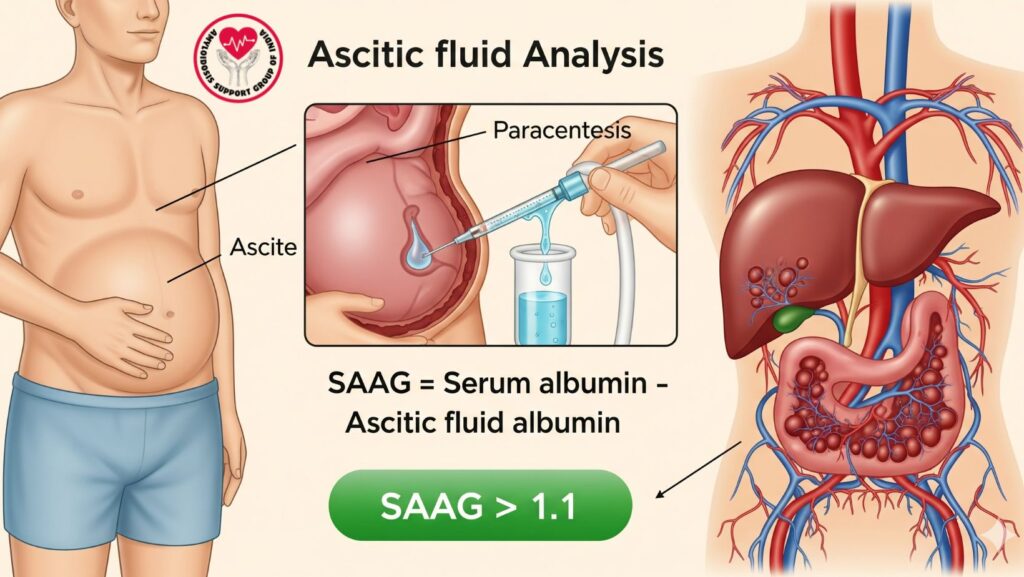
Table of Contents
Introduction
Ascites, or the collection of fluid in the peritoneal cavity, is a frequent complication of liver disease and other systemic illnesses. Accurate ascitic fluid evaluation is necessary to identify its underlying etiology, which directs appropriate treatment.
One of the most important parameters in ascitic fluid analysis is the serum-ascites albumin gradient (SAAG). A SAAG >1.1 g/dL is strongly suggestive of portal hypertension as a cause for ascites. Familiarity with the mechanisms, interpretation, and clinical implications of SAAG is important for clinicians who care for patients with liver disease, heart failure, or other systemic illnesses.
This in-depth guide covers:
- Physiology and pathophysiology of ascites
- Serum-ascites albumin gradient (SAAG) principles
- Etiology and ascites types
- Diagnostic workup, such as laboratory, imaging, and invasive methods
- Clinical implication of SAAG >1.1
- Treatment approaches for portal hypertensive ascites
- Real-world case studies and applications
- Emerging trends in ascites assessment and research
Physiology of Ascitic Fluid Formation
Normal Fluid Dynamics
- The peritoneal cavity holds a small amount of lubricating fluid (~50 mL).
- There is fluid exchange among capillaries, lymphatics, and peritoneal mesothelium.
- Balance of hydrostatic and oncotic pressures determines fluid accumulation.
Mechanisms Causing Ascites
- Portal hypertension: Elevated hydrostatic pressure in hepatic sinusoids forces fluid into the peritoneal space.
- Hypoalbuminemia: Decreased plasma oncotic pressure predisposes to fluid leakage.
- Peritoneal inflammation: Infection or malignancy elevates vascular permeability.
- Lymphatic obstruction: Malignancy or fibrosis prevents fluid drainage.
Serum-Ascites Albumin Gradient (SAAG)
Definition
- SAAG = Serum albumin – Ascitic fluid albumin
- Derived from concurrent ascitic fluid and serum samples
Interpretation
- SAAG >1.1 g/dL: Points towards portal hypertension (increased hydrostatic pressure in hepatic circulation).
- SAAG <1.1 g/dL: Points towards non-portal hypertension causes (peritoneal carcinomatosis, infections such as TB, pancreatitis).
Physiologic Basis
- Portal hypertension leads to transudation of fluid poor in albumin, resulting in elevated SAAG.
- Non-portal hypertension causes exudative ascites with elevated protein content, resulting in low SAAG.
Causes of Ascites
Ascites with SAAG >1.1 (Portal Hypertension)
- Cirrhosis (most common)
- Cardiac ascites (right heart failure, constrictive pericarditis)
- Budd-Chiari syndrome (hepatic vein obstruction)
- Sinusoidal obstruction syndrome
Ascites with SAAG <1.1 (Non-Portal Hypertension)
- Peritoneal carcinomatosis
- Tuberculous peritonitis
- Nephrotic syndrome
- Pancreatic ascites
- Hypoalbuminemia without portal hypertension
Diagnostic Evaluation of Ascites
Clinical Assessment
- History: Alcohol use, viral hepatitis, heart failure, malignancy
- Physical examination: Shifting dullness, fluid wave, peripheral edema, hepatomegaly
Laboratory Tests
- SAAG calculation: Central diagnostic step
- Total protein in ascitic fluid: Distinguishes cardiac vs cirrhotic ascites
- Cell count and differential: Identify infection (spontaneous bacterial peritonitis)
- Culture and cytology: Recognize pathogens or malignant cells
Imaging Studies
- Ultrasound: Ascertains ascites, liver size, portal vein flow
- CT/MRI: Assesses underlying causes (tumors, fibrosis, vascular obstruction)
- Echocardiography: Explores cardiac causes of ascites
Invasive Techniques
- Paracentesis: Necessary for fluid analysis
- Hepatic vein catheterization: Records portal pressure
- Liver biopsy: Assesses for cirrhosis, fibrosis, or infiltrative disease
Clinical Implication of SAAG >1.1
- Separates portal hypertension from other etiologies
- Directs treatment plans: diuretics, paracentesis, or management of underlying cardiac/hepatic illness
- Aids prognostic prediction in liver disease: increased SAAG usually indicates more severe complications
Association with Liver Disease Severity
- High SAAG and low ascitic fluid protein: Imply cirrhotic ascites, increased risk of spontaneous bacterial peritonitis
- High SAAG and high ascitic fluid protein: Imply cardiac ascites or Budd-Chiari syndrome
Management of Ascites Due to Portal Hypertension
General Principles
- Sodium restriction (2 g/day)
- Fluid restriction if hyponatremia present
- Weight and abdominal girth monitoring
Pharmacologic Therapy
- Diuretics:
- Spironolactone first-line
- Furosemide for combination therapy
- Albumin infusion: Avoids circulatory dysfunction during large-volume paracentesis
Interventional Procedures
- Large-volume paracentesis: Relief of symptoms
- Transjugular intrahepatic portosystemic shunt (TIPS): Refractory ascites
- Liver transplantation: Cirrhosis with portal hypertension, definitive therapy
Complication Management
- Spontaneous bacterial peritonitis (SBP): Prophylactic antibiotics in high-risk patients
- Hepatorenal syndrome: Vasoconstrictors and albumin therapy
- Electrolyte imbalance: Measure potassium, sodium, renal function
Case Studies
- Patient A: Ascites due to cirrhosis and SAAG 1.5 g/dL, improved symptomatically with diuretics and paracentesis.
- Patient B: Cardiac ascites due to right heart failure, SAAG 1.3 g/dL, improved with optimized heart failure therapy.
- Patient C: Budd-Chiari syndrome, SAAG 1.4 g/dL, improved with TIPS procedure and portal pressures and ascites resolution.
Special Considerations
Refractory Ascites
- Defined as ascites not responding to standard therapy
- Demands TIPS, liver transplant, or palliative therapy
Ascites in Systemic Diseases
- Amyloidosis, nephrotic syndrome, pancreatic disease can have intricate fluid profiles
- SAAG continues to be important in separating portal hypertension from other causes
Prognostic Implications
- Recurrent ascites with elevated SAAG suggests advanced portal hypertension
- Early detection enables prompt intervention, reduction in risk, and treatment of complications
Future Directions
*
- Biomarkers: Developing new serum or urine biomarkers for the detection of early portal hypertension
- Non-invasive imaging: MRI and elastography for portal pressure measurement
- Personalized therapy: SAAG-guided, liver function-optimized, and comorbidity-adapted interventions
- Systemic disease research: Ascites mechanisms in AL amyloidosis and related conditions
Clinical Pearls
- SAAG is better than total protein in separating ascites etiology.
- SAAG >1.1 g/dL is highly suggestive of portal hypertension, irrespective of ascitic protein concentration.
- Identification of portal hypertension’s underlying cause is crucial for directed therapy.
- Repeated or refractory ascites needs to be multidisciplinary managed, involving hepatology, cardiology, and interventional radiology.
Conclusion
A serum-ascites albumin gradient (SAAG) >1.1 g/dL is an important diagnostic marker of portal hypertension as the etiology of ascites. Ascertaining proper evaluation of ascitic fluid, along with clinical, laboratory, and imaging evaluation, allows:
- Effective differentiation between portal hypertension and non-portal hypertension causes
- Recognition of the underlying disease (cirrhosis, heart failure, vascular obstruction)
- Directed management, such as diuretics, paracentesis, TIPS, and liver transplantation
- Prognostication and surveillance of complications
Clinicians may take SAAG into account in all patients with ascites in order to achieve early intervention, better outcomes, and optimal care.

