Prognosis of AL Amyloidosis Patients with Jaundice – Median Survival and Clinical Implications
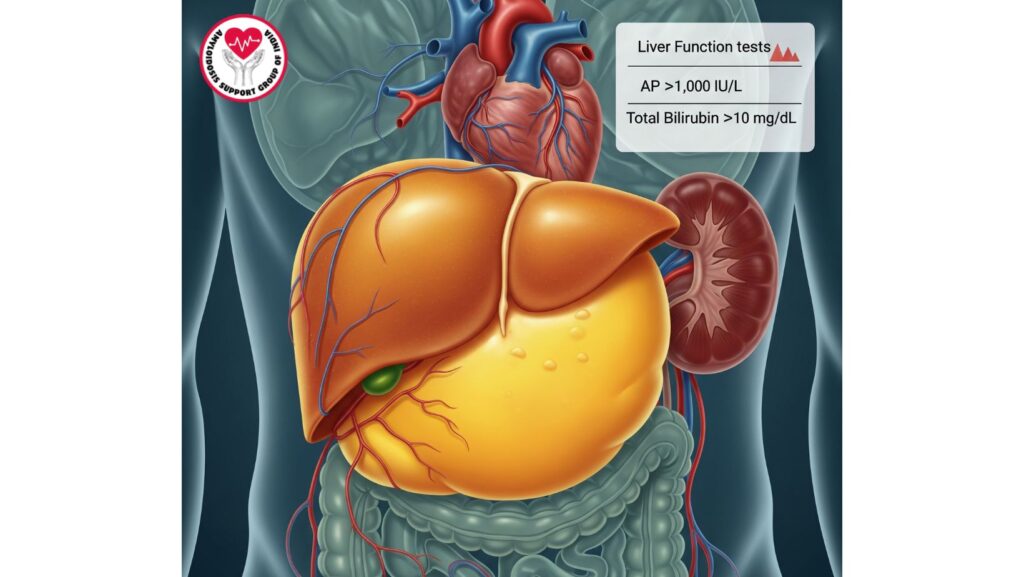
Table of Contents
Introduction
Systemic primary (AL) amyloidosis is a multisystem disorder of rare occurrence due to the deposition of misfolded immunoglobulin light chains. Although the liver is affected in 60–90% of patients, the majority are subclinical with minimal liver function test abnormalities and hepatomegaly.
Despite this, the jaundice onset in AL amyloidosis is a turning point, indicating severe cholestatic liver disease. Median survival following the onset of jaundice is roughly 3 months, according to studies, and reflects the acute severity of hepatic amyloidosis in this subgroup.
Knowledge of prognostic significance, clinical manifestations, diagnostic approach, and management is vital for physicians, caregivers, and patients alike to make informed choices and ensure proper care.
Epidemiology and Risk Factors
Prevalence
- Clinically significant jaundice in AL amyloidosis is rare and presents in a minority of patients (~5–10%) with hepatic involvement.
- The majority of the patients are older adults with an age range of 55–70 years.
Risk Factors for Severe Hepatic Involvement
- Multisystem high burden of amyloid
- Acute progression of amyloid deposition
- Highly amyloidogenic light chain subtypes
- Underlying renal or cardiac compromise, which can amplify liver impairment
Pathophysiology
Mechanisms Contributing to Jaundice
- Amyloid deposition in sinusoids impairs liver cell function.
- Obstruction of bile by amyloid infiltration of portal tracts and bile canaliculi.
- Vascular impairment compromises hepatic perfusion, which aggravates hepatocellular injury.
- Combined multi-organ involvement underlies systemic manifestations like hypoalbuminemia, ascites, and edema.
Cholestatic Liver Failure in AL Amyloidosis
- Severe cholestasis is the major cause of jaundice.
- Synthetic function of the liver is impaired, resulting in coagulopathy and hypoalbuminemia.
- Sudden worsening differentiates this subgroup from patients with mild, subclinical liver disease.
Clinical Features
Hepatic Signs
- Jaundice: Frequently the initial obvious sign of severe hepatic involvement
- Hepatomegaly: Tender or nontender enlargement of the liver
- Pruritus: Secondary to cholestasis
- Ascites: Secondary to portal hypertension and hypoalbuminemia
Laboratory Findings
- Total bilirubin: Typically greatly elevated (>10 mg/dL)
- Alkaline phosphatase: Typically >1,000 IU/L
- AST/ALT: Mild-to-moderate increases
- Albumin: Reduced due to hepatic dysfunction or nephrotic syndrome
- INR: Prolonged due to impaired synthetic capacity
Systemic Manifestations
- Fatigue, anorexia, edema
- Cardiac involvement: arrhythmias, heart failure
- Renal involvement: worsening proteinuria or renal failure
Diagnostic Approach
Laboratory Evaluation
- LFTs and coagulation profile for hepatic function assessment
- Serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) to detect monoclonal light chains
- Serum free light chain assay to quantify amyloidogenic proteins
Imaging
- Ultrasound: Hepatomegaly, heterogeneous echotexture
- CT/MRI: Nodular liver, ascites, portal hypertension
Liver Biopsy
- Definitive diagnosis: Congo red staining shows apple-green birefringence under polarized light
- Mass spectrometry: Confirms AL type
- Transjugular biopsy: Ideal in coagulopathy or ascites
Prognostic Implications
- Median survival following onset of jaundice: ~3 months
- Poor prognosis indicators:
- Total bilirubin >10 mg/dL
- Alkaline phosphatase >1,000 IU/L
- Acute decline in hepatic synthetic function
- Multi-organ disease
Impact of Multi-Organ Disease
- Coincident cardiac amyloidosis augments mortality
- Renal impairment will exacerbate hypoalbuminemia and ascites
- Systemic disease burden commonly excludes transplantation
Management Strategies
Medical Therapy
- Plasma cell-directed therapy:
- Bortezomib, cyclophosphamide, dexamethasone, or daratumumab
- Supportive care:
- Diuretics for ascites
- Nutritional support
- Management of pruritus
Advanced Interventions
- Liver transplantation: Exceptional, only in solitary hepatic disease
- Combined organ transplantation: Only for highly selected patients
Palliative Care
- Emphasis on symptom control, comfort, and quality of life
- Early integration is advised in severe disease
- Part of treatment includes management of pruritus, ascites, fatigue, and psychological support
Case Studies and Literature Review
- Case 1: Presenting with jaundice, hepatomegaly, and increased AP. Multi-organ involvement made transplant impossible; median survival after jaundice 3 months.
- Case 2: Sudden onset jaundice with renal and cardiac amyloidosis; patient expired on hospice within 4 weeks.
- Case 3: Exceptional isolated hepatic AL amyloidosis; liver transplant successfully performed; patient survived >2 years after procedure.
Clinical Pearls
- Jaundice in AL amyloidosis is an influential prognostic indicator of extensive hepatic involvement.
- Median survival is roughly 3 months, and so urgency for treatment and palliative planning is emphasized.
- Early diagnosis by biopsy and mass spectrometry is necessary to manage.
- Multidisciplinary care enhances outcomes with systemic disease.
- Supportive and palliative measures integration is crucial to quality of life.
Future Directions
- New therapies aimed at hepatic amyloid deposits
- Development of biomarkers for early identification of high-risk patients
- Clinical trials investigating transplantation approaches and combination treatments
- Advanced imaging modalities to track liver progression in systemic AL amyloidosis
Conclusion
Presence of jaundice in AL amyloidosis indicates severe cholestatic liver failure and grim prognosis, with a median survival of around 3 months. Identification of this subset is important for:
- Prognostication
- Systemic therapy guidance
- Palliative therapy planning
Key Takeaways: - The majority of AL amyloidosis patients have mild or subclinical liver disease.
- Jaundice is an indicator of a high-risk group with accelerated disease progression.
- Multidisciplinary and palliative care interventions are needed to maximize outcomes.
Comprehensive management strategies and early detection can enhance patient care and quality of life even in this high-risk subgroup.

