Prognosis for AL Amyloidosis
The outlook for AL amyloidosis varies greatly based on how early the disease is found, which organs are affected, and how well the patient responds to treatment. Heart involvement is the biggest factor in a negative outcome. Patients with severe heart damage often have a shorter life expectancy, sometimes less than a year if untreated. However, recent improvements in treatment, including chemotherapy and autologous stem cell transplantation, have significantly increased survival for many patients. Those diagnosed early and who achieve a complete blood response may live for 10 years or more.
Kidney involvement is serious but generally more manageable and does not reduce life expectancy as much as heart problems. Overall, the median survival ranges from less than one year in advanced stages to over seven years in early stages. Ongoing research and new treatments continue to provide hope, especially for patients diagnosed early and treated at specialized centers.
Table of Contents
1. Introduction
2. What Is AL Amyloidosis?
3. Why Prognosis Varies So Widely
4. Key Prognostic Factors
5. Staging Systems and Their Impact on Prognosis
6. Treatment Options and Their Influence on Outcomes
7. Median Survival Rates
8. Organ-Specific Prognosis
9. Impact of Early vs Late Diagnosis
10. Quality of Life and Functional Outcomes
11. Remission, Relapse, and Long-Term Management
12. Living with AL Amyloidosis
13. Current Research and Hope for the Future
14. Conclusion
Introduction
- AL (light chain) amyloidosis is a rare and complex disorder where misfolded light chain proteins from abnormal plasma cells build up as amyloid fibrils in various tissues and organs. These deposits disrupt normal function, often affecting the heart, kidneys, liver, nerves, and gastrointestinal system.
- The prognosis for AL amyloidosis** has been traditionally poor, especially when diagnosed late or when multiple organs are involved. However, **improvements in early detection, chemotherapy, and stem cell transplantation** have greatly enhanced patient outcomes.
- This article discusses the prognosis of AL amyloidosis in detail, covering the factors that influence it, how it’s measured, and how patients can manage their treatment and outlook.
2. What Is AL Amyloidosis?
- AL amyloidosis occurs due to the overproduction of **immunoglobulin light chains** by abnormal plasma cells. These light chains misfold and create insoluble fibrils that deposit in tissues and organs.
- This leads to: Organ dysfunction ,Systemic inflammation ,Progressive deterioration if untreated .
- The kidneys and heart are usually the most affected, but the nervous system, liver, and gastrointestinal tract can also be involved. The degree and pattern of organ involvement significantly impact prognosis.
3. Why Prognosis Varies So Widely
- No two cases of AL amyloidosis are identical. Prognosis differs based on several factors, including .
- Number of organs involved.
- Severity of organ damage (especially cardiac).
- Speed of diagnosis .
- Effectiveness of treatment .
- Patient age and overall health .
- Patients diagnosed early with minimal organ involvement and who respond well to treatment generally have a better outlook than those diagnosed late with severe cardiac or renal damage.
4. Key Prognostic Factors
1. Cardiac Involvement
- This is the most crucial prognostic factor. Amyloid infiltration of the heart leads to restrictive cardiomyopathy , arrhythmias, and heart failure. Elevated biomarkers like NT-PROBNP and troponin suggest a poor prognosis.
2. Renal Function
- When amyloid impacts the kidneys, the patient may experience proteinuria, nephrotic syndrome, or renal failure. The level of renal dysfunction at diagnosis influences survival and quality of life.
3. Hematologic Response
- Patients who respond well to chemotherapy—particularly those who achieve complete hematologic remission (CR) tend to have significantly better outcomes.
4. Age and Comorbidities
- Older patients or those with other health issues (like diabetes or hypertension) often have a harder time with treatment, which can affect outcomes.
5. Staging Systems and Their Impact on Prognosis
- Different staging systems classify the severity of the disease and predict survival.
- Mayo 2004 Staging System:
- This system relies on:
- NT-PROBNP (>332 ng/L)
- Troponin T (>0.035 ng/mL)
Stages:
Stage I : No elevated markers (best prognosis)
Stage II: One elevated marker
Stage III: Both elevated (poor prognosis)
Mayo 2012 Revised Staging System:
This system adds a third marker: difference between involved and uninvolved free light chains (DFLC) .
This 4-stage system provides a more detailed prognosis and helps guide treatment decisions.
6. Treatment Options and Their Influence on Outcomes
- Chemotherapy
- Regimens like CYBORD (cyclophosphamide, bortezomib, dexamethasone) or Daratumumab-based treatments focus on reducing light chain production. Patients who respond well may see improvements in organ damage and longer survival.
- Autologous Stem Cell Transplantation (ASCT)
- For certain patients (usually younger and with minimal cardiac involvement), ASCT can lead to long-term remission. However, not every patient qualifies for this treatment.
- Supportive Care
- Managing fluid balance, heart failure, kidney dysfunction, and nutritional needs is essential for improving quality of life and treatment tolerance.
7. Median Survival Rates
- Survival has improved significantly over the last two decades. Still, it varies based on disease stage and response to treatment .Overall Median Survival:
Stage I: 7–10 years
Stage II: 4–5 years Stage IIIA: 2 years
Stage IIIB: 1 year Patients Achieving Complete Response (CR)
- Median survival often exceeds 10 years
- Early diagnosis and effective treatment can greatly improve survival rates.
8. Organ-Specific Prognosis
- Cardiac Amyloidosis
- This is the most vital factor in survival.
Patients with advanced cardiac involvement** may survive only 6–12 months without effective treatment.
- With CR and cardiac response, survival improves significantly.
- Neurological Amyloidosis
- It progresses more slowly.
- Symptoms can affect quality of life but have less effect on survival.
- Renal Amyloidosis
- Kidney failure might necessitate dialysis.
- This does not immediately reduce life expectancy if managed properly.
- A renal transplant is possible after achieving remission.
9. Impact of Early vs. Late Diagnosis
- Early: diagnosis is crucial.
- Early: Better organ function, higher treatment tolerance, and greater chance of hematologic response.
- Late: Irreversible damage, limited treatment options, lower survival rates.
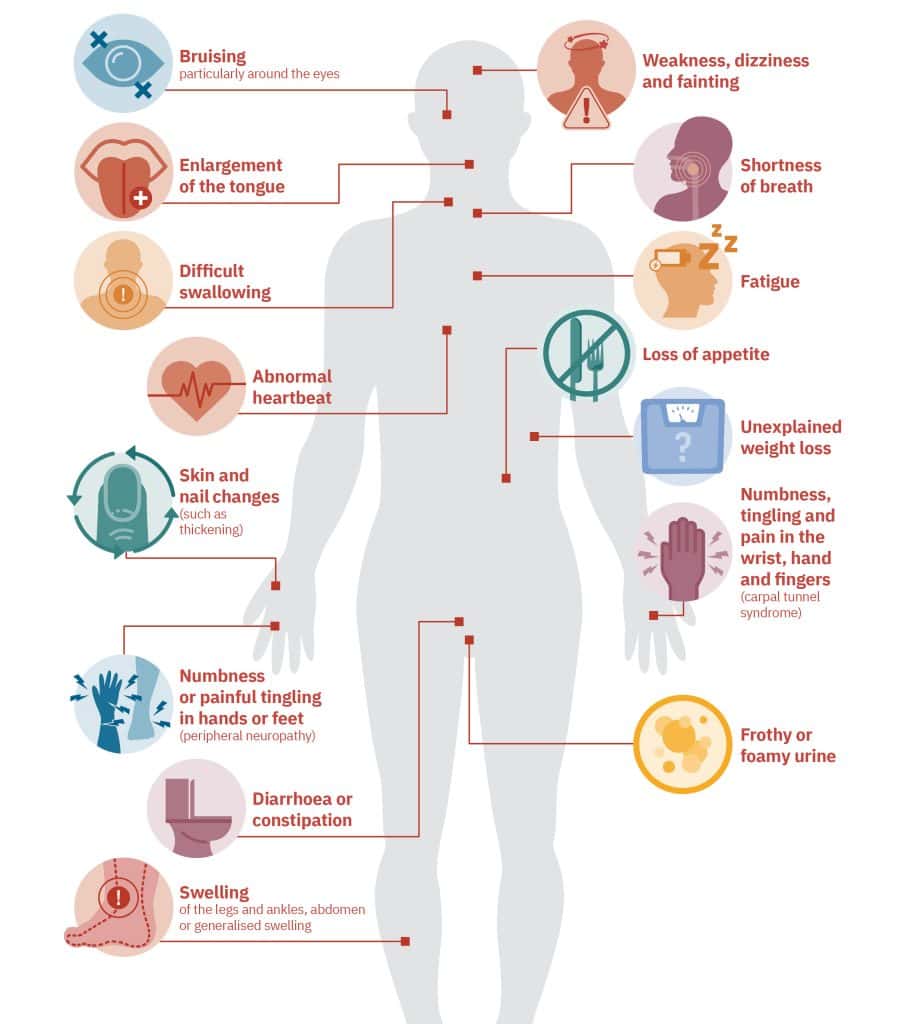
- Sadly, the non-specific symptoms (fatigue, weight loss, swelling) can delay diagnosis by months. Raising awareness among clinicians and patients is essential for early detection.
10. Quality of Life and Functional Outcomes
- Prognosis is not just about survival. It’s also about how well patients live.
- Patients in remission may experience:
- Improved organ function (especially heart and kidneys)
- Less fatigue and pain
- Better physical mobility
- Emotional and psychological recovery
However, on going challenges may include:
- Peripheral neuropathy
- Remaining heart damage
- Emotional stress and anxiety about relapse
- Financial burdens
Comprehensive care involving cardiology, nephrology, oncology, dietetics, and mental health is crucial for better outcomes.
11. Remission, Relapse, and Long-Term Management
Complete Remission (CR)
- This is characterized by the absence of detectable light chains and improvement in organ function.
- CR is the best predictor of long-term survival.
- Relapse
- AL amyloidosis can reappear after months or years.
- Monitoring includes regular blood and urine tests and observing biomarkers.
- Maintenance Therapy
This isn’t commonly used, but current research is exploring its role for high-risk patients.
12. Living with AL Amyloidosis
- Receiving an AL amyloidosis diagnosis can change a person’s life, but many patients continue to lead fulfilling lives. Key strategies include:
- Regular follow-ups with specialists
- Lifestyle changes (diet, exercise, hydration)
- Mental health support to address anxiety or depression
- Participating in support groups for connection and empowerment
13. Current Research and Hope for the Future
- Exciting research is underway to enhance outcomes for AL amyloidosis, such as:
- Monoclonal antibodies targeting amyloid deposits
- New drug combinations that are easier to tolerate
- CAR-T cell therapy being tested in clinical trials
- Organ regeneration and support therapies
With advancements in early detection methods (like biomarker screening and AI diagnostic tools), future patients may receive a diagnosis before organ damage happens .a potential game changer for prognosis.
14. Conclusion
The prognosis for AL amyloidosis has significantly improved due to early detection and better treatments. While the disease remains serious—particularly when there is heart involvement—many patients can achieve long-term remission and enjoy a good quality of life.
- The main factors that impact prognosis include:
- Level of organ damage at diagnosis.
- Patient’s response to treatment.
- Age and other health issues.
- Access to skilled, interdisciplinary care.
If you or someone you care about has been diagnosed with AL amyloidosis, remember that you are not alone. With expert guidance, timely therapy, and proper support, there is genuine hope for substantial recovery.

