Prophylactic Anticoagulation in Nephrotic Syndrome: When and Why It’s Needed”
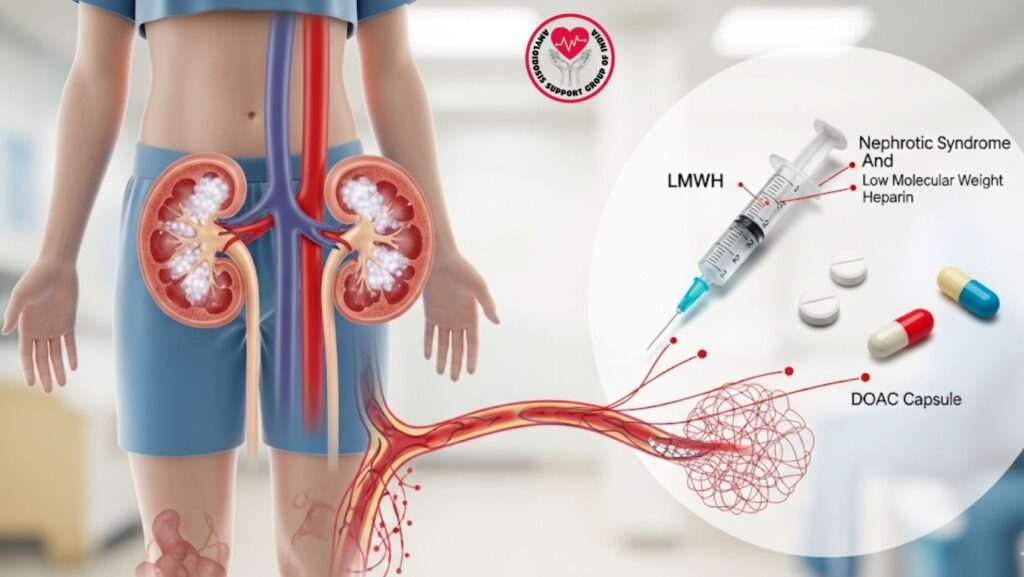
Table of Contents
1. Introduction
Nephrotic syndrome is defined by severe proteinuria, hypoalbuminemia, hyperlipidemia, and edema. Among the major complications is a heightened susceptibility to thromboembolism, most of all venous thromboembolism (VTE) and, to a lesser extent, arterial events.
Prophylactic anticoagulation may minimize thrombotic risk but must be carefully weighed against risk of bleeding. Available evidence indicates that patients with serum albumin <20 g/L and other risk factors (e.g., immobility, previous thrombosis, or severe heart disease) derive maximum benefit.
This article discusses the pathophysiology of thrombosis in nephrotic syndrome, indications for prophylaxis, anticoagulant options, monitoring, and outcome, giving a readable manual for clinicians and patients.
2. Pathophysiology of Nephrotic Syndrome Thrombosis
2.1 Hypercoagulable State
Nephrotic syndrome is a risk factor for thrombosis because of:
- Excretion of anticoagulant proteins in the urine (antithrombin III, protein C, protein S)
- Overproduction of procoagulant factors (fibrinogen, factor VIII)
- Hyperactivity and aggregation of platelets
- Hemoconcentration from diuretics or hypovolemia
2.2 Risk Factors
- Severe hypoalbuminemia (<20 g/L)
- Prolonged immobilization
- Prior history of thrombosis
- Concurrent infection or inflammation
- Cardiac disease (particularly atrial fibrillation)
Case Example:
A 58-year-old man with AL amyloidosis and nephrotic-range proteinuria (serum albumin 18 g/L) presented with a deep vein thrombosis (DVT). Subsequent patients with the same risk profiles were given prophylactic anticoagulation, with prevention of thrombotic events.
3. Indications for Prophylactic Anticoagulation
3.1 Albumin Threshold
- Serum albumin <20 g/L is an important marker of hypercoagulability
- Risk rises exponentially as the albumin level falls
3.2 Other Risk Factors
- History of prior thrombotic events
- Severe immobility or hospitalization
- Concurrent cardiac disease
- Volume depletion due to high-dose diuretics or nephrotic syndrome
Clinical Tip:
Prophylaxis individualized with consideration of thrombotic vs. bleeding risk.
4. Anticoagulant Choice
4.1 Low-Molecular-Weight Heparin (LMWH)
- Most commonly utilized for short-term prophylaxis
- Dosing with respect to body weight and renal function
- Benefit: predictable anticoagulation and minimal monitoring needs
4.2 Warfarin
- Utilized for prolonged prophylaxis
- Needs INR monitoring (target of 2–3 in most patients)
- Can be impacted by hypoalbuminemia, with dose titration needed
4.3 Direct Oral Anticoagulants (DOACs)
- Comprise apixaban, rivaroxaban, dabigatran
- Sparse information in nephrotic syndrome, but increasing evidence in favour of its use in selected patients
- Benefits: oral therapy, no regular monitoring
5. Dosing Strategies and Duration
- Short-term prophylaxis: LMWH during admission or acute illness
- Long-term prophylaxis: Warfarin or DOACs for patients with chronic severe hypoalbuminemia
- Adjustments of dose: Indicated in renal impairment or varying albumin level
- Re-evaluation: Periodically review bleeding risk and risk of thrombosis
Case Example:
A patient with albumin 17 g/L and immobility was given LMWH for 10 days when hospitalized, with subsequent switching to apixaban for continued prophylaxis. There were no thrombotic events during 6 months.
6. Monitoring During Anticoagulation
- In LMWH: Monitor anti-Xa level in renal impairment or extreme body weight
- For Warfarin: Routine INR monitoring
- For DOACs: Follow kidney function and bleeding signs
- Clinical evaluation: Look for bruising, hematuria, gastrointestinal bleeding, or epistaxis
7. Risks and Adverse Effects
- Bleeding (major and minor)
- Heparin-induced thrombocytopenia (HIT) with unfractionated heparin
- Drug interactions: Especially with warfarin
- Over-anticoagulation: Needs very careful monitoring of INR or anti-Xa
Clinical Tip:
Trade off thrombosis prevention with bleeding risk, particularly in patients with advanced amyloidosis or co-morbidities.
8. Integration with Other Nephrotic Syndrome Therapies
- RAS blockers: Can decrease proteinuria and indirectly decrease thrombotic risk
- Diuretics: Regulate edema, but lead to hemoconcentration
- Disease-specific therapy: Chemotherapy in AL amyloidosis, anti-inflammatory therapy in AA amyloidosis
- Combination approach: Prophylactic anticoagulation adds value to other treatments to minimize complications
9. Case Studies and Real-World Outcomes
- Case 1: 60-year-old man with AL amyloidosis, albumin 18 g/L, immobile; prophylaxis with LMWH avoided DVT in hospital
- Case 2: 55-year-old woman with AA amyloidosis, albumin 19 g/L, on long-term diuretics; warfarin averted thromboembolism within 12 months
- Observation: Prophylaxis markedly lowers VTE incidence in high-risk patients, especially those with albumin <20 g/L
10. Patient Education and Lifestyle
- Teach symptoms of thrombosis: swelling, pain, shortness of breath
- Stress compliance with anticoagulation therapy
- Promote mobility and leg exercises
- Educate about bleeding risk and precautions (e.g., shaving, avoiding trauma)
11. Future Directions
- Studies on DOAC efficacy and safety in nephrotic syndrome
- Personalized thrombosis vs. bleeding risk scoring
- Integration with new amyloidosis and CKD therapies to mitigate hypercoagulability
12. Conclusion
Prophylactic anticoagulation is a life-saving intervention for nephrotic syndrome patients with severe hypoalbuminemia (<20 g/L) and other thrombotic risk factors.
Cautious selection, monitoring, and integration with other therapies can avoid life-threatening thromboembolic complications and reduce bleeding complications. Early identification and risk stratification enhance patient outcomes and quality of life.

