Case Report: Sudden Progression of Liver Disease – MELD Score Rise from 14 to 29 in a 61-Year-Old Patient
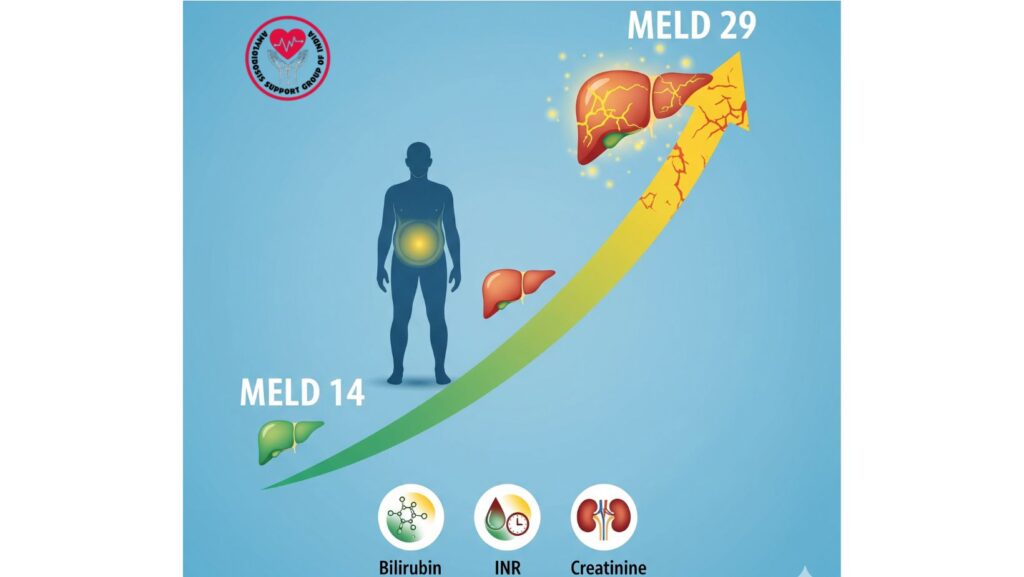
Table of Contents
Introduction
Liver disease worsening is usually tracked by using validated scoring systems, and the Model for End-Stage Liver Disease (MELD) score has emerged as a vital prognostic indicator in clinical practice. Herein, we report a 61-year-old patient with systemic amyloidosis who initially came to the medical attention for abdominal distension, lower limb edema, and worsening liver function. During the course of his disease, the patient’s MELD score went dramatically up from 14 to 29, indicating quickening clinical worsening.
This article examines the case at length, highlighting the MELD score’s utility in assessing the severity of disease, prognosis, and directing therapeutic intervention, particularly in complicated cases like amyloidosis.
Case Presentation
Initial Symptoms
The patient had:
- Subacute swelling of the lower extremities and abdomen over a period of two months.
- Fatigue, decreased appetite, and abdominal pain.
- No history of alcoholism, viral hepatitis, or autoimmune liver disease.
Physical Examination Findings
- Bilateral lower extremity edema
- Tense ascites
- Jugular venous distention
These findings indicated portal hypertension and systemic fluid overload.
Laboratory Investigations
On First Admission
- Albumin: 2.1 g/dL (hypoalbuminemia)
- AP: 718 IU/L
- AST: 158 IU/L
- ALT: 119 IU/L
- Total Bilirubin (TB): 0.5 mg/dL
- INR: 1.07
- Creatinine: 0.9 mg/dL
- Urine analysis: Nephrotic-range proteinuria
Viral and autoimmune panels (ANA, ASMA, AMA, Hepatitis B and C) were normal, excluding secondary causes.
Imaging
- Abdominal CT: Ascites, potentially nodular liver, no hepatosplenomegaly.
- Transthoracic echocardiogram: Left ventricular hypertrophy, suspicious for infiltrative disease.
Diagnostic Procedures
- Sigmoid colon biopsy → Congo red staining positive for amyloid.
- Mass spectrometry → AL amyloidosis diagnosed.
Readmission and Disease Progression
A month post-discharge, the patient was readmitted with:
- Worsening ascites
- New-onset jaundice
Repeat Liver Function Tests
- Total Bilirubin: 21.6 mg/dL
- AP: 1317 IU/L
- AST: 260 IU/L
- ALT: 104 IU/L
These results suggested severe cholestasis and progressive hepatic dysfunction.
Liver Biopsy
- Transjugular liver biopsy was done because ascites was present.
- Amyloidosis without inflammation, granulomas, fibrosis, or malignancy was confirmed by histopathology.
MELD Score Assessment
Initial MELD Score
- MELD 14 → moderate risk of mortality, stable at presentation.
*
On Readmission
- MELD 29 → high risk of mortality within 3 months.
This sudden upsurge accentuates the accelerated development of liver failure in systemic amyloidosis, reflecting the unfavorable prognosis in late stages.
Discussion
What is the MELD Score?
The MELD score (Model for End-Stage Liver Disease) is utilized to:
- Estimate 90-day mortality in advanced liver disease patients.
- Direct prioritization for liver transplantation.
- Follow disease progression objectively.
It is calculated based on:
- Bilirubin
- INR
- Creatinine
- (Occasionally sodium, in MELD-Na score)
Clinical Relevance in This Case
- The patient’s MELD score increased from 14 to 29 in under two months, with rapid decompensation.
- Elevated bilirubin and deteriorating ascites were major factors.
- Although there was no malignancy or major fibrosis present, amyloid infiltration led to extreme liver dysfunction.
Prognostic Considerations
- MELD 14: Indicates moderate survival probability, usually manageable with medical treatment.
- MELD 29: Suggests urgent liver transplant consideration (albeit candidacy is complicated by systemic amyloidosis).
- Progression is rapid in AL amyloidosis with multiorgan involvement.
Management Strategies
Supportive Treatment
- Diuretics for ascites (spironolactone, furosemide).
- Restriction of salt and monitoring of fluid balance.
- Paracentesis for tense ascites.
Specific to Amyloidosis
- Chemotherapy (e.g., bortezomib, cyclophosphamide, dexamethasone) aimed at plasma cell dyscrasia.
- Stem cell transplantation in suitable candidates.
- Multidisciplinary care by hepatology, nephrology, cardiology, and hematology.
Transjugular Liver Biopsy Role
- Diagnostic procedure with a safe option in patients with ascites.
- Provided histopathologic confirmation without causing bleeding.
Case Lessons
- Amyloidosis may imitate chronic liver disease with ascites, jaundice, and enzyme disturbance.
- Monitoring the MELD score is crucial when showing rapid progression.
- Abrupt MELD rise (14 → 29) indicates severe deterioration and poor prognosis.
- Even in the absence of fibrosis or malignancy, functional impairment from amyloid infiltration can be tragic.
- Multiorgan assessment is paramount—cardiac, renal, and hepatic involvement deteriorate survival.
Conclusion
This example of a 61-year-old patient with AL amyloidosis is an illustration of the catastrophic evolution of liver disease, as attested by a MELD score rise from 14 to 29 in weeks. It emphasizes the prognostic value of MELD scoring, the diagnostic value of transjugular liver biopsy, and the need for multidisciplinary management of systemic amyloidosis urgently.
For clinicians, this report emphasizes that normal biopsy results in terms of malignancy or fibrosis do not rule out severe hepatic dysfunction in cases of amyloidosis. Early diagnosis, close follow-up, and early referral for advanced treatment continue to be key to improving outcomes.

