Case Report: Sigmoid Colon Biopsy as a Diagnostic Tool for Amyloidosis in a 61-Year-Old Patient
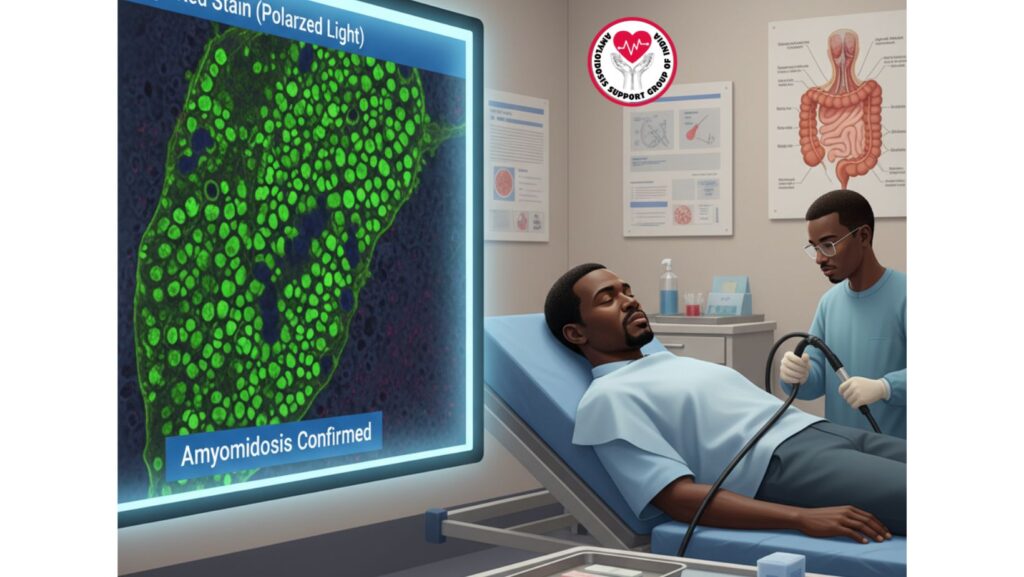
Table of Contents
Introduction
Amyloidosis is a rare systemic illness with the extracellular deposition of misfolded protein fibrils within multiple organs and tissues. Diagnosis usually demands a high degree of suspicion, especially if patients have multisystem involvement like nephrotic-range proteinuria, ascites, and restrictive cardiomyopathy signs.
Although multiple biopsy sites can be used to establish amyloidosis, such as bone marrow, fat pad, kidney, and liver, on this occasion a sigmoid colon biopsy yielded the final histopathological diagnosis. This paper describes the clinical course of a 61-year-old African-American man in whom a colon biopsy established systemic amyloidosis, highlighting the choice of site for tissue sampling in difficult cases.
Patient Background
The patient complained of a two-month history of progressive abdominal distension and bilateral lower limb edema. Clinical assessment showed:
- Bilateral lower limb edema
- Tense ascites
- Jugular venous distension
Laboratory tests were: - Hypoalbuminemia (2.1 g/dL)
- Elevated alkaline phosphatase (718 IU/L)
- AST (158 IU/L) and ALT (119 IU/L)
- Normal total bilirubin (0.5 mg/dL)
- Normal INR (1.07) and creatinine (0.9 mg/dL)
- Nephrotic-range proteinuria
Autoimmune and viral panels were negative. Imaging showed ascites with potential nodular liver changes but no hepatosplenomegaly. Echocardiogram showed concentric left ventricular hypertrophy suspicious for an infiltrative process.
Suspicion for systemic amyloidosis at this point was high, and tissue biopsy was necessary to make the diagnosis.
Why Biopsy Is Essential in Amyloidosis Diagnosis
Final diagnosis of amyloidosis needs histological proof. Laboratory and imaging results might be compatible with amyloidosis, but only biopsy with special staining can identify amyloid fibril deposition.
The stains most often employed are:
- Congo red stain – shows the pathognomonic apple-green birefringence under polarized light.
- Crystal violet or thioflavin T – other staining techniques.
Biopsy makes diagnosis and typing of amyloidosis possible, which directs treatment planning (e.g., AL or ATTR amyloidosis).
Why the Sigmoid Colon Was Selected
Biopsy locations in suspected amyloidosis differ based on patient presentation and risk factors. The sigmoid colon is a convenient location because:
- It is readily accessible with colonoscopy.
- The colon will frequently exhibit vascular and submucosal amyloid deposits.
- It is associated with lower risk than more invasive biopsies like cardiac or hepatic sampling.
- GI biopsy amyloidosis sensitivity rates are between 50–70% in systemic disease.
A sigmoid colon biopsy was chosen in this patient, as the patient already had ascites and systemic features, so colonoscopy was a safe and viable possibility.
Histopathological Findings
The sigmoid colon biopsy showed:
- Amorphous eosinophilic deposits within the submucosa and vessel walls.
- Congo red staining positive, which demonstrates classical apple-green birefringence under polarized light.
- Results in keeping with systemic amyloidosis.
This confirmed the clinical suspicion and permitted directed management to start.
Differential Diagnosis Before Biopsy
Prior to the biopsy findings, differential diagnoses were:
- Cirrhosis with portal hypertension
- Nephrotic syndrome due to non-amyloid causes (e.g., membranous nephropathy, diabetic nephropathy)
- Heart failure with preserved ejection fraction
- Malignancy-associated ascites
The negative ascitic fluid cytology and sterile culture excluded infection and malignancy. The biopsy eventually proved amyloidosis as the underlying unifying diagnosis.
Role of Sigmoid Colon Biopsy in Literature
Some studies have underscored the usefulness of gastrointestinal biopsies in systemic amyloidosis:
- GI biopsies have been able to identify amyloid deposits in patients with nephrotic syndrome or hepatic involvement, even in the absence of GI symptoms.
- The sensitivity is variable but frequently circumvents the requirement for more invasive biopsies.
- A positive result is very specific for amyloidosis, particularly if confirmed by immunohistochemistry or mass spectrometry for amyloid typing.
Management After Diagnosis
1. Amyloid Typing
Following confirmation, identification of AL amyloidosis versus ATTR amyloidosis is paramount.
- AL amyloidosis necessitates investigation of plasma cells (bone marrow biopsy, serum free light chains).
- ATTR amyloidosis involves transthyretin misfolding and is hereditary or wild-type.
2. Systemic Management
- Diuretics for ascites and edema.
- Salt and fluid restriction.
- Supportive therapy for renal and hepatic involvement.
3. Targeted Therapy
- AL amyloidosis: Chemotherapy (bortezomib, cyclophosphamide, dexamethasone), potential stem cell transplant.
- ATTR amyloidosis: Tafamidis, patisiran, or diflunisal.
4. Multidisciplinary Approach
- Cardiology for infiltrative cardiomyopathy.
- Nephrology for renal support.
- Hematology for systemic treatment in AL amyloidosis.
Prognosis and Follow-Up
The prognosis is based on:
- Amyloidosis type (AL vs ATTR)
- Organ involvement extent (cardiac, renal, hepatic)
- Therapeutic response
Early diagnosis through sigmoid colon biopsy enabled this patient to initiate prompt therapy, increasing likelihood of stabilizing disease course.
Conclusion
This case highlights the value of tissue biopsy in making a diagnosis of systemic amyloidosis. Although numerous sites are available for biopsy, the sigmoid colon biopsy was an effective and safe diagnostic procedure in this 61-year-old patient. The results not only made the diagnosis but also directed additional workup and treatment.
In clinical practice, to include colonic biopsy in the diagnostic algorithm for amyloidosis is of great worth, particularly in those with systemic manifestations but with noncontributory lab and imaging results.

