Supportive Care in Advanced Hepatic Amyloidosis: Controlling Symptoms and Complications
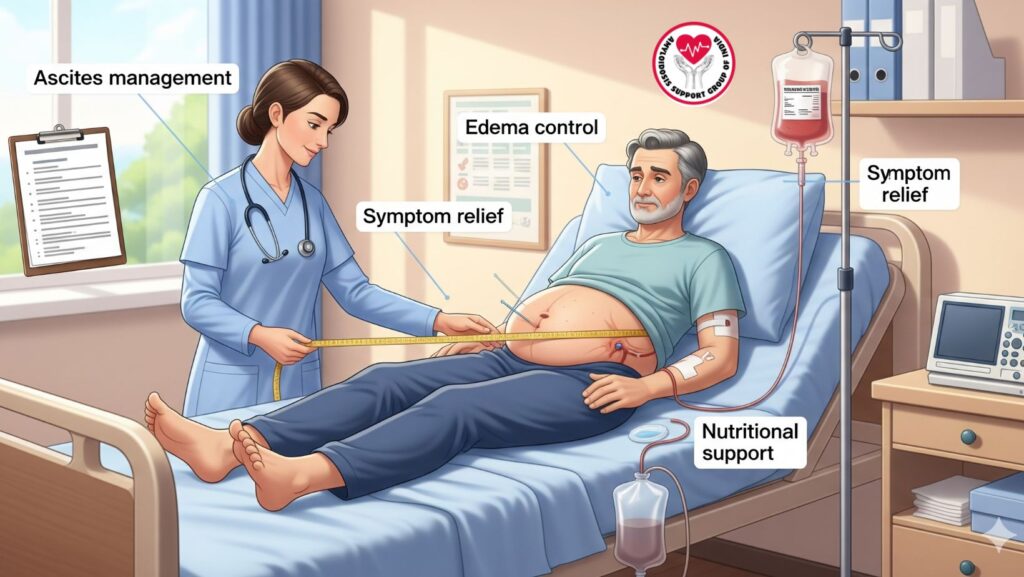
Table of Contents
Introduction
Advanced hepatic amyloidosis is a fulminant form of systemic amyloidosis in which amyloid deposits interfere with liver function, resulting in complications such as ascites, edema, and fatigue. Though disease-directed treatments (chemotherapy, stem cell transplantation) address amyloid synthesis, supportive care is essential to preserve patient comfort, quality of life, and organ function.
This article addresses evidence-based supportive care approaches, such as ascites, edema management, nutritional management, symptom control, and palliative care.
1. Understanding Advanced Hepatic Amyloidosis
- Definition: Extensive amyloid deposition in liver tissue resulting in structural and functional compromise.
- Clinical findings: Hepatomegaly, jaundice, ascites, peripheral edema, fatigue, and pruritus.
- Laboratory results: Elevation of alkaline phosphatase (ALP), mild elevation of transaminases, gradual increase in bilirubin, hypoalbuminemia.
- Complications: Portal hypertension, coagulopathy, malnutrition, and eventual liver failure.
Key Point: Supportive care emphasizes symptom relief and management of complications, in addition to disease-specific treatment.
2. Ascites Management
Ascites is a frequent complication in advanced hepatic amyloidosis secondary to portal hypertension and hypoalbuminemia.
2.1 Evaluation
- Physical exam: Abdominal distension, shifting dullness, fluid wave
- Ultrasound: Establishes fluid accumulation and excludes other causes
- Lab work: Serum albumin, renal function, electrolytes
2.2 Non-Pharmacologic Interventions
- Sodium restriction: Restrict daily intake to 2g–3g
- Fluid management: Monitor intake, particularly in hyponatremic patients
- Regular monitoring: Monitor abdominal girth and weight
2.3 Pharmacologic Therapy
- Diuretics:
- Spironolactone (aldosterone antagonist) – first-line
- Furosemide (loop diuretic) – add if inadequate response
- Dose titration: Gradually adjust to avoid renal impairment or electrolyte disturbance
2.4 Procedural Interventions
- Paracentesis: Therapeutic drainage of large-volume ascites
- Frequently done with albumin infusion to avoid hypotension
- Transjugular intrahepatic portosystemic shunt (TIPS): Infrequently applied, only for selected refractory instances
Objective: Enhance comfort, mobility, and breathing function.
3. Edema Management
Peripheral edema occurs due to hypoalbuminemia and portal hypertension.
3.1 Non-Pharmacologic Interventions
- Leg elevation: Decreases dependent edema
- Compression stockings: Beneficial if venous insufficiency is present
- Weight monitoring: Early identification of fluid retention
3.2 Pharmacologic Management
- Diuretics: Same drugs as for ascites (spironolactone ± furosemide)
- Check renal function and electrolytes to prevent complications
3.3 Nutritional Considerations
- Ensure good protein intake for albumin production
- Restrict excessive salt intake to prevent fluid overload
Key Point: Edema control enhances mobility, skin integrity, and quality of life.
4. Nutritional Support
Malnutrition in advanced hepatic amyloidosis is frequent due to anorexia, malabsorption, and protein loss.
4.1 Assessment
- Body mass index (BMI)
- Serum albumin and prealbumin
- Dietary intake and caloric assessment
4.2 Recommendations
- Small, frequent meals that are high in protein and calories
- Oral supplements if oral intake is not sufficient
- Vitamin supplementation: Fat-soluble vitamins (A, D, E, K) secondary to cholestasis
- Enteral feeding: In patients unable to take enough by mouth
Objective: Preserve muscle mass, immunity, and overall functional status.
5. Symptom Management
5.1 Pruritus
- Frequent secondary to bile salt accumulation
- Management:
- Cholestyramine (binds bile acids)
- Antihistamines for symptomatic relief
- Topical emollients for skin comfort
5.2 Fatigue and Weakness
- Promote light activity and rest balance
- Treat underlying causes: anemia, malnutrition, or sleep disturbances
5.3 Pain Management
- Usually mild, but analgesics may be necessary
- Avoid hepatotoxic drugs (e.g., high-dose acetaminophen)
- Use opioids with caution if liver function is greatly impaired
5.4 Jaundice and Skin Care
- Moisturizers for dry skin
- Photoprotection to reduce pruritus and irritation
6. Monitoring and Follow-Up
Regular follow-up is necessary:
- Laboratory tests: LFTs, renal function, electrolytes, coagulation profile
- Imaging: Ultrasound for ascites or liver changes
- Symptom monitoring: Edema, ascites, fatigue, pruritus
- Review of medications: Diuretic dosing, nutritional supplements, supportive medications
Objective: Early recognition of complications and timely adjustment of supportive care.
7. Palliative and End-of-Life Considerations
For patients with severe hepatic amyloidosis not candidates for disease-modifying therapy:
- Comfort focus: Manage pain, pruritus, ascites, and edema
- Advanced care planning: Explore prognosis, goals of care, and patient preference
- Multidisciplinary care: Palliative care, hepatology, nutrition support, and nursing care
- Psychosocial support: Family and patient counseling
Outcome: Improves quality of life and dignity in advanced stages of disease.
8. Case Example: Supportive Care in Advanced Hepatic Amyloidosis
Patient: 63-year-old man with AL amyloidosis, hepatomegaly, and ascites
Interventions:
- Sodium restriction and diuretics for edema and ascites
- Frequent, small high-protein feeds with supplements
- Cholestyramine and emollients for pruritus
- Intermittent laboratory monitoring and ultrasound follow-up
Outcome: - Enhanced comfort, mobility, and symptom management
- Disease-directed therapy continued concomitantly
Clinical Relevance: Illustrates the effect of supportive care on the quality of life in patients.
9. Summary Table: Supportive Care Strategies
| Complication | Supportive Measures | Goal |
| ———— | ———————————————– | ——————————————- |
| Ascites | Sodium restriction, diuretics, paracentesis | Minimize pain and abdominal distension |
| Edema | Leg elevation, compression, diuretics | Enhance mobility and prevent skin breakdown |
| Malnutrition | Enteral feeding, supplements, high-protein diet | Preserve immune status and muscle mass |
| Pruritus | Antihistamines, emollients, cholestyramine | Enhance comfort |
| Fatigue | Rest-activity balance, treat underlying causes | Improve daily function |
| Pain | Safe analgesics, avoid hepatotoxic drugs | Reduce discomfort |
| Jaundice | Skin care, monitor liver function | Minimize irritation |
10. Conclusion
Supportive care in late hepatic amyloidosis is essential for symptom management, enhancing quality of life, and augmenting disease-directed treatment.
Key Takeaways:
- Edema and ascites demand procedural, pharmacologic, and dietary management.
- Nutrition therapy resists malnutrition and maintains functional status.
- Control of symptoms (pruritus, fatigue, pain) improves comfort and well-being.
- Careful monitoring and multidisciplinary treatment are needed for best outcomes.
- Palliative strategies are crucial when disease-modifying treatment is impossible.

