Understanding Systemic Amyloidosis: Causes, Organ Involvement, and Clinical Impact
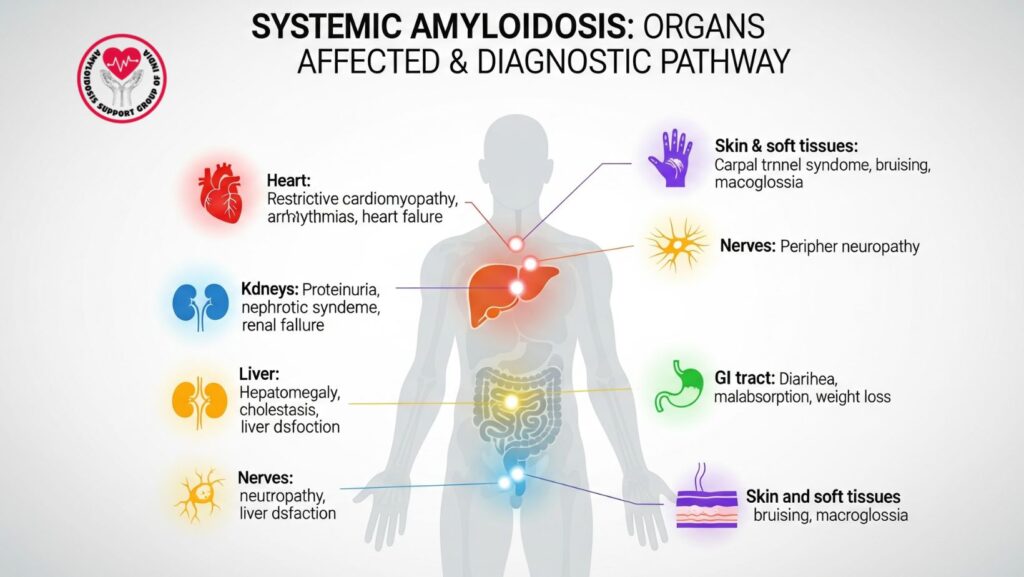
Table of Contents
1. Introduction
Systemic amyloidosis is a serious but rare disorder caused by the deposition of misfolded proteins, or amyloid fibrils, in various organs of the body. The condition may affect various systems at the same time and lead to progressive organ dysfunction, organ failure, and death if untreated.
Although amyloidosis is deemed rare, its clinical significance is increasing, as an increasing number of cases are being identified thanks to better diagnostic tools like mass spectroscopy and newer imaging modalities. The trick for clinicians lies in earlier detection and prompt treatment, as the prognosis in most cases rests on how early the disease is identified and whether or not damage to organs can be reversed or prevented.
2. What is Systemic Amyloidosis?
Systemic amyloidosis is a set of protein misfolding diseases in which soluble precursor proteins destabilize, misfold, and convert to insoluble fibrils. These fibrils are deposited in essential organs like the heart, kidneys, liver, nerves, and gastrointestinal tract.
- Systemic vs. localized amyloidosis:
- Systemic amyloidosis → affects more than one organ and has diffuse effects.
- Localized amyloidosis → limited to a single organ or tissue (e.g., localized bladder amyloidosis, laryngeal amyloidosis).
Key Insight: Systemic amyloidosis is much more perilous than localized types because it causes multi-organ dysfunction and significant mortality if left untreated.
3. Types of Systemic Amyloidosis
There are various types of systemic amyloidosis, divided by the precursor protein involved:
3.1 AL (Light Chain) Amyloidosis
- Due to misfolded immunoglobulin light chains secreted by plasma cell dyscrasias (e.g., multiple myeloma).
- Most prevalent type in developed nations.
- Organs affected: heart, kidneys, liver, peripheral nerves.
3.2 AA (Secondary) Amyloidosis
- Develops as a complication of chronic inflammatory diseases (e.g., rheumatoid arthritis, tuberculosis, Crohn’s disease).
- Etiology: serum amyloid A protein deposition.
- Affects mainly the kidneys and liver.
3.3 ATTR (Transthyretin) Amyloidosis
- Due to deposition of misfolded transthyretin protein (liver-secreted).
- Two forms:
- Hereditary ATTR (TTR gene mutations).
- Wild-type ATTR (age-related, prevalent in older men, formerly referred to as senile systemic amyloidosis).
- Principally involves the heart and nerves.
3.4 Other Rare Forms
- Aβ2M amyloidosis (dialysis-associated).
- Apolipoprotein AI amyloidosis.
- Gelsolin amyloidosis.
4. Causes and Pathophysiology
Systemic amyloidosis is basically a protein misfolding disorder.
- Step 1: Some precursor proteins (light chains, serum amyloid A, transthyretin) lose stability.
- Step 2: These proteins misfold to form β-pleated sheet structures.
- Step 3: Misfolded proteins aggregate to form insoluble fibrils.
- Step 4: Amyloid fibrils accumulate in organs → disrupt normal structure → impair organ function.
Pathophysiological Consequences: - Organ stiffness and enlargement.
- Vascular fragility resulting in bleeding.
- Impaired organ metabolism and function.
5. Organs Commonly Affected in Systemic Amyloidosis
Amyloid deposition may be in any organ except the brain. Most commonly affected are:
- Heart: Restrictive cardiomyopathy, arrhythmias, heart failure.
- Kidneys: Nephrotic syndrome, proteinuria, progressive renal failure.
- Liver: Hepatomegaly, cholestasis, elevated alkaline phosphatase.
- Nervous system: Peripheral neuropathy, autonomic dysfunction.
- GI tract: Diarrhea, malabsorption, weight loss.
- Skin & soft tissues: Carpal tunnel syndrome, easy bruising, periorbital purpura.
6. Clinical Features and Symptoms
6.1 General Symptoms
- Fatigue
- Unintentional weight loss
- Weakness
6.2 Organ-Specific Symptoms
- Cardiac: Dyspnea, edema, arrhythmias, syncope.
- Renal: Swelling, frothy urine, renal failure.
- Liver: Enlarged liver, jaundice, abdominal discomfort.
- Neurologic: Numbness, tingling, orthostatic hypotension.
- GI: Diarrhea, constipation, malabsorption.
- Skin: Bruising around the eyes (raccoon eyes), thickened tongue (macroglossia).
Key Insight: Amyloidosis is very often characterized by non-specific symptoms, and therefore is delayed in diagnosis.
7. Diagnostic Approach
7.1 Clinical Suspicion
- Unexplained heart failure, kidney disease, or liver dysfunction should prompt concern.
**7.2 Laboratory Tests
- Serum and urine protein electrophoresis.
- Serum free light chain assay.
- Immunofixation for monoclonal proteins.
7.3 Imaging Studies
- Echocardiography (restrictive cardiomyopathy).
- Cardiac MRI (amyloid infiltration patterns).
- Ultrasound/CT/MRI for hepatomegaly.
7.4 Biopsy
- Congo red staining → apple-green birefringence under polarized light.
7.5 Protein Typing
- Mass spectroscopy → gold standard for amyloid protein type identification.
8. Prognosis and Complications
- Untreated systemic amyloidosis is progressive and fatal.
- Median survival varies by type:
- AL amyloidosis with cardiac involvement: <1 year if untreated.
- ATTR amyloidosis: Progression slower, survival to 5–10 years.
- Major complications: heart failure, renal failure, hepatic failure, severe neuropathy.
9. Treatment Approaches
9.1 AL Amyloidosis
- Chemotherapy: Bortezomib, cyclophosphamide, dexamethasone.
- Stem cell transplant: In suitable patients.
9.2 AA Amyloidosis
- Manage underlying inflammatory disease (e.g., biologics in RA, antibiotics in TB).
9.3 ATTR Amyloidosis
- Tafamidis (TTR stabilizer).
- Patisiran and Inotersen (gene-silencing therapies).
- Liver transplant for hereditary types.
10. Supportive Care Measures
- Cardiac: Diuretics, judicious fluid management.
- Renal: End-stage disease dialysis.
- Hepatic: Relief from jaundice, control of ascites.
- Neuropathy: Pain management, physiotherapy.
- Nutrition: High-protein diet, supplementation.
11. Living with Systemic Amyloidosis
Patients may need lifestyle modifications:
- Low-salt diet in the setting of heart/renal involvement.
- Monitoring of kidney and liver function on a regular basis.
- Physiotherapy in neuropathy.
- Psychological support for managing chronic illness.
12. Future Directions and Research
- New amyloid-targeting antibodies in the pipeline.
- Gene-silencing drugs for ATTR with encouraging results.
- Advanced imaging devices for early detection of organ involvement.
13. Key Takeaways for Clinicians and Patients
- Systemic amyloidosis = multi-organ disease with high mortality if left untreated.
- Early diagnosis is vital for survival.
- Biopsy + mass spectroscopy are critical for proper typing.
- Individualized therapy by type (AL, AA, ATTR) enhances results.
- Supportive and palliative care are essential for quality of life.
14. Conclusion
Systemic amyloidosis is a potentially lethal protein misfolding disease that can involve almost every organ in the body. For clinicians, the most important message is to think about amyloidosis in patients with unexplained organ dysfunction—particularly of the heart, kidneys, or liver.
Early identification, precise protein typing, and early institution of disease-specific therapy can revolutionize the outcome for patients, holding out promise for a previously untreatable illness.

