Case Report: Transjugular Liver Biopsy in a 61-Year-Old Patient with Severe Hepatic Dysfunction
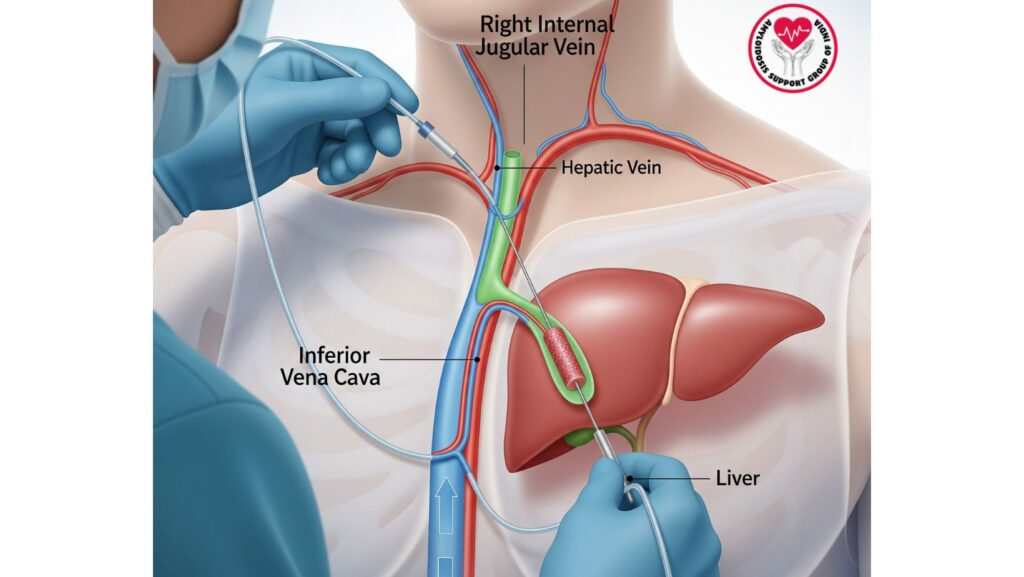
Table of Contents
Introduction
Liver biopsies continue to be a standard in the diagnosis of liver ailments. For those with advanced liver dysfunction, percutaneous biopsy is fraught with great danger, especially because of coagulopathy, portal hypertension, and ascites. For such patients, the transjugular liver biopsy (TJLB) offers a safer and valuable option.
This case presentation is of a 61-year-old African-American man with primary AL amyloidosis who had presenting symptoms of progressive hepatic failure, jaundice, and ascites. Upon his readmission, a transjugular liver biopsy was done to define the nature and extent of liver involvement.
The case highlights:
- Why TJLB was preferred over percutaneous techniques
- How the biopsy had invaluable diagnostic insights
- The wider role of TJLB in the management of patients with end-stage systemic amyloidosis
Patient Background
Initial Presentation
The patient presented initially with:
- Subacute abdominal and lower extremity swelling (more than 2 months)
- Bilateral lower extremity edema
- Tense ascites
- Jugular venous distention
Key Laboratory Findings (First Admission)
- Albumin: 2.1 g/dL (hypoalbuminemia)
- AP: 718 IU/L (elevated)
- AST: 158 IU/L
- ALT: 119 IU/L
- Total Bilirubin: 0.5 mg/dL (normal)
- Creatinine: 0.9 mg/dL (normal renal function)
- Urinalysis: Nephrotic range proteinuria
**Workup and Diagnosis
- CT Scan: Ascites, probable nodular liver
- SAAG: >1.1 (portal hypertension)
- Echocardiogram: Left ventricular hypertrophy (potential infiltrative cardiomyopathy)
- Sigmoid Colon Biopsy: Positive for amyloid deposits
- Mass Spectroscopy: Established primary AL amyloidosis
Readmission and Clinical Deterioration
One Month Later
The patient was readmitted with:
- Progressive ascites
- New jaundice
Repeat Laboratory Values
- Total Bilirubin: 21.6 mg/dL (severe increase)
- AP: 1317 IU/L (severe elevation)
- AST: 260 IU/L
- ALT: 104 IU/L
These results implied severe hepatic dysfunction and progressive amyloid infiltration of the liver.
Decision for Transjugular Liver Biopsy (TJLB)
Why Not Percutaneous Biopsy?
- High bilirubin and liver dysfunction raised risk of bleeding.
- Ascites rendered percutaneous biopsy unsafe.
- Portal hypertension added procedural risk.
Why Transjugular Biopsy Was Appropriate
- TJLB permits biopsy via the internal jugular vein → hepatic veins → liver tissue.
- If there is bleeding, it escapes into the venous system and decreases risk of intraperitoneal bleeding.
- Safest procedure for patients with coagulopathy, ascites, or severe hepatic dysfunction.
Procedure: Transjugular Liver Biopsy
Steps Involved
- Access via the right internal jugular vein under local anesthesia and ultrasound control.
- Advancement of the catheter into the hepatic vein under fluoroscopy.
- Insertion of the biopsy needle through the catheter into the liver parenchyma.
- Multiple tissue cores taken for histopathological assessment.
Advantages in This Patient
- No peritoneal puncture → decreased risk of bleeding
- Safe even with ascites
- Sufficient diagnostic tissue acquired
Histopathology Results
The transjugular liver biopsy demonstrated:
- Widespread amyloid deposition within the hepatic parenchyma and sinusoids
- Hepatocyte compression secondary to infiltrative process
- Compatible with hepatic amyloidosis secondary to AL amyloidosis
This proved that the patient’s progressing jaundice and ascites were caused by progressive hepatic infiltration by amyloid fibrils.
Clinical Discussion
Significance of TJLB in Hepatic Amyloidosis
- Offers definitive tissue diagnosis when clinical and imaging results are uncertain.
- Best method in patients with ascites, coagulopathy, or portal hypertension.
- Enables histologic confirmation and correlation with systemic amyloidosis.
Prognostic Implications
- High-grade hyperbilirubinemia (>20 mg/dL) and widespread amyloid infiltration suggest poor prognosis.
- Median survival from jaundice onset is frequently shorter than 6 months.
- Systemic treatment (chemotherapy) is usually restricted due to liver failure.
Comparison with Other Cases in Literature
- Research by Gertz and Kyle describes TJLB as priceless in the diagnosis of amyloidosis, especially in case other biopsy sites are negative or uninformative.
- Case series have demonstrated TJLB to possess high diagnostic yield with low complication rates even in advanced disease.
Management and Outcome
Supportive Care
- Large-volume paracentesis for ascites
- Albumin infusions
- Nutritional support
- Diuretics as tolerated
Limitations of Therapy
- Advanced hepatic dysfunction made aggressive chemotherapy impossible.
- Care was changed to palliative focus, with emphasis on symptom control and quality of life.
Key Learning Points
- Transjugular liver biopsy is the gold standard in patients with advanced hepatic dysfunction, ascites, or coagulopathy.
- Percutaneous biopsy would have been unsafe in this patient.
- Histology confirmed hepatic amyloidosis, correlating with severe jaundice and elevated liver enzymes.
- Prognosis is poor once bilirubin exceeds 20 mg/dL in amyloidosis patients.
- Multidisciplinary care consisting of hepatology, hematology, cardiology, and palliative care is a must.
Conclusion
This is a case of a 61-year-old patient with AL amyloidosis illustrating the important role of transjugular liver biopsy in the diagnosis of advanced hepatic involvement. The procedure was safe in the face of ascites and extreme liver dysfunction, and it established amyloid infiltration to be responsible for the increasing jaundice.
The observations emphasize that:
- TJLB is the preferred biopsy in high-risk patients.
- Liver involvement with bilirubin >20 mg/dL has a dismal prognosis.
- Prompt diagnosis and treatment of amyloidosis are critical prior to hepatic decompensation.
This case is a useful clinical vignette for those who treat systemic amyloidosis with liver involvement, reinforcing the importance of timely biopsy and thorough patient management.

