Understanding the MELD Score: Determining Chronic Liver Disease Severity and Transplant Priority
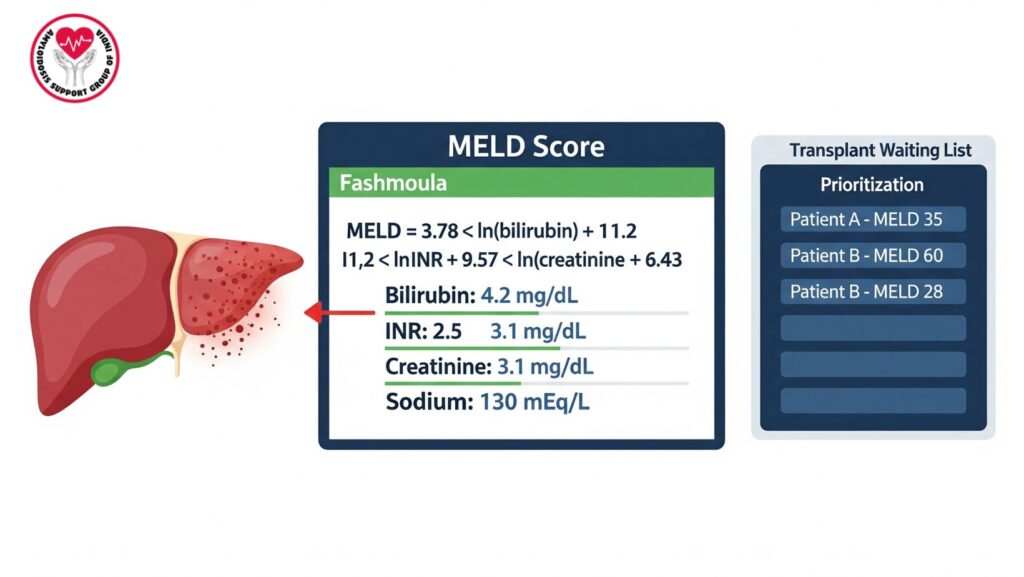
Table of Contents
Introduction
Chronic liver disease constitutes a significant global health burden, frequently advancing insidiously to late stages. Clinicians use objective scoring systems to measure disease severity, forecast survival, and direct treatment. Of these tools, the Model for End-Stage Liver Disease (MELD) score has emerged as the standard against which prognosis and priority for liver transplantation are measured.
This thorough guide describes the history, calculation, clinical utility, limitations, and changing role of the MELD score in hepatology and transplant medicine.
1. What is the MELD Score?
- Definition: The MELD score is a scoring system initially created to estimate survival in patients receiving transjugular intrahepatic portosystemic shunt (TIPS).
- Current Role: Widely utilized to evaluate the severity of chronic liver disease and distribute donor livers equitably.
- Scoring Range: 6 (mildest) to 40 (severest). Higher scores = increased risk of mortality.
2. Parameters Included in MELD Score
The MELD score takes four laboratory parameters into account:
- Serum Bilirubin – indicates the liver function to excrete bile.
- International Normalized Ratio (INR) – evaluates blood coagulation and liver synthetic function.
- Serum Creatinine – evaluates kidney function, important because renal impairment aggravates the prognosis.
- Serum Sodium (MELD-Na update) – decreased sodium signifies poorer outcomes.
3. Formula for MELD Score
The standard formula:
$$
MELD = 3.78 \times \ln(\text{bilirubin}) + 11.2 \times \ln(\text{INR}) + 9.57 \times \ln(\text{creatinine}) + 6.43
$$
- Creatinine is truncated at 4.0 mg/dL.
- Any value <1.0 is reset to 1.0 to prevent negative results.
- MELD-Na: MELD + 1.59 × (135 – sodium).
4. Clinical Applications of MELD Score
4.1 Prognosis in Cirrhosis
- Forecasts 90-day mortality risk.
- Greater MELD → worse survival if not transplanted.
4.2 Liver Transplant Allocation
- MELD ensures objective and equitable organ allocation.
- More ill patients (more points) are placed higher on waiting list.
4.3 Treatment Planning
- Determines timing of procedures (TIPS, transplant, palliative care).
5. MELD Score Ranges and Mortality Risk
*
- <9: 1.9% 3-month mortality.
- 10–19: 6% mortality.
- 20–29: 20% mortality.
- 30–39: 52.6% mortality.
- ≥40: 71% mortality.
6. MELD vs Child-Pugh Score
- Child-Pugh: Clinical parameters (ascites, encephalopathy) + labs.
- MELD: Laboratory-based only, more objective.
- Current Practice: MELD preferred for transplant listing.
7. Strengths of MELD Score
- Objective, reproducible, evidence-based.
- Good predictor of short-term survival.
- Standardized across transplant centers.
8. Limitations of MELD Score
- May underestimate in:
- Patients with refractory ascites.
- Hepatocellular carcinoma (HCC).
- Severe cholestasis.
- Does not explicitly measure quality of life or complications such as variceal bleeding.
9. MELD Exceptions
- Certain conditions are awarded “exception points” to compensate for MELD limitations:
- Hepatocellular carcinoma.
- Hepatopulmonary syndrome.
- Certain metabolic liver disorders.
10. Evolution of MELD – MELD-Na and Beyond
- MELD-Na: Adds serum sodium, enhancing predictive validity.
- Future Models: MELD 3.0 incorporates female sex and albumin.
- Ongoing investigation into the use of imaging and genetic biomarkers.
11. Case Example – Use of MELD Score
- Patient: 61-year-old with ascites and jaundice.
- Labs: Bilirubin 21.6, INR 1.8, Creatinine 1.5, Sodium 128.
- MELD-Na:
~34 → High risk, urgent transplant need.
12. Prognosis and Outcomes Based on MELD
- Low MELD: Can delay transplant, monitor conservatively.
- Moderate MELD: Optimize treatment, list for transplant.
- High MELD: Prioritize urgent transplantation.
13. MELD in Research and International Transplant Policy
- Used by UNOS (United States), Eurotransplant, and other liver networks.
- Enhances fairness and results over previous systems.
- AI-assisted survival prediction models under investigation.
14. Patient Education – MELD Awareness
Patients should be aware:
- MELD is not a reflection of how ill they “feel,” but of chance of survival.
- It assists in determining when transplantation is most advantageous.
- Lifestyle interventions (alcohol abstinence, diet, medication compliance) may control disease while on the waiting list.
15. Future Directions
- Incorporation with imaging biomarkers (MRI, elastography).
- Genetic and proteomic risk stratification.
- AI-based individualized transplant allocation.
Conclusion
The MELD score transformed hepatology and transplant medicine, rendering organ allocation more objective and fair. Through the integration of bilirubin, INR, creatinine, and sodium, it offers a consistent measure of chronic liver disease prognosis. Although not perfect, MELD is still the foundation of liver transplantation decision-making globally.

