Table of Contents
What Are the Main Causes of AL Amyloidosis?
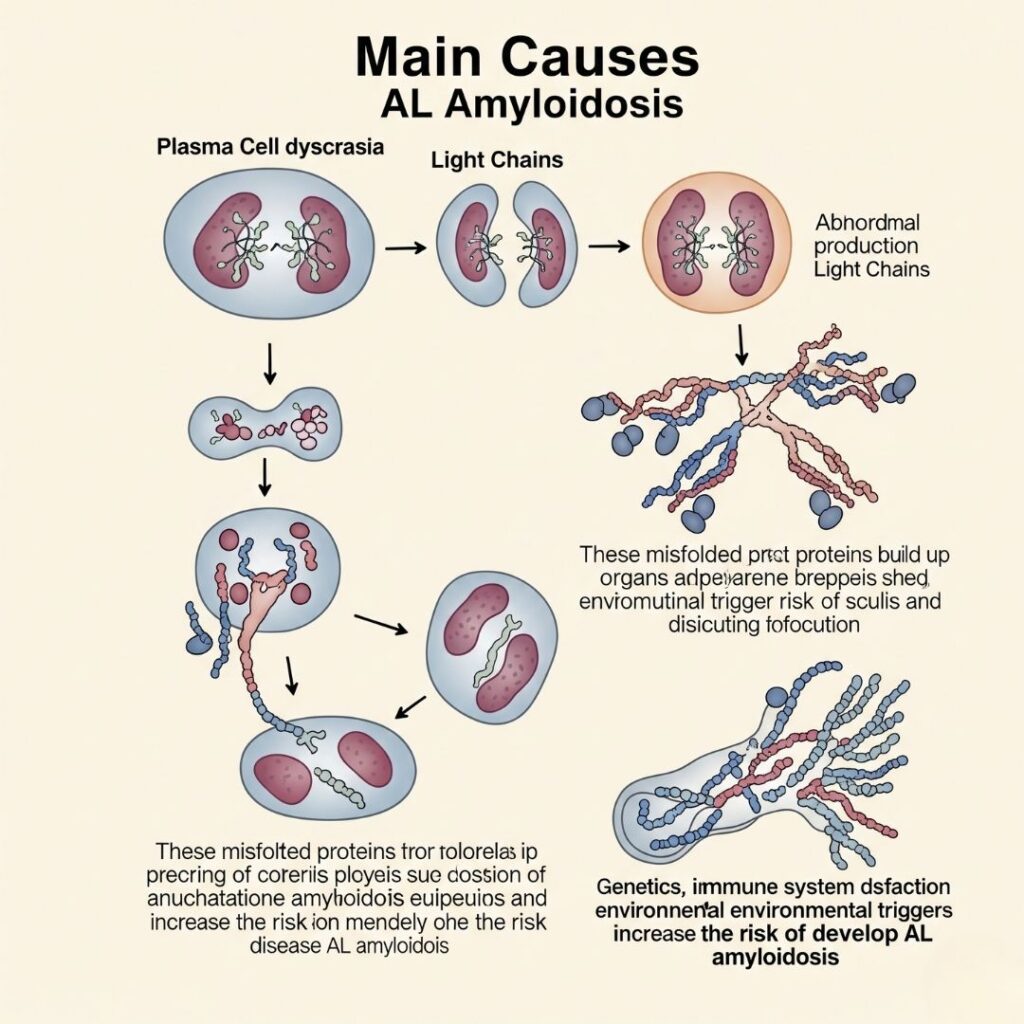
AL amyloidosis, or Primary Amyloidosis, is a serious but rare condition that occurs when aberrant plasma cells generate proteins that are misfolded and undergo formation of amyloid fibrils. The fibrils are deposited in organs and tissues, which causes their dysfunction. With increasing awareness of rare diseases, it’s critical to know the root causes of AL amyloidosis for facilitating early diagnosis and effective treatment.
This ultimate guide by amyloidosissupport delves into the causes, risk factors, pathophysiology, and initiating conditions of AL amyloidosis and gives practical insights into prevention, early diagnosis, and care.
What Is AL Amyloidosis?
Its is a bone marrow disorder in which plasma cells secrete a misfolded variant of light chains (one of the building blocks of antibodies). These aberrantly folded light chains aggregate to become amyloid proteins that circulate and deposit in important organs such as the heart, kidneys, liver, nerves, and gastrointestinal tract.
It is referred to as “AL” since the fibrils are made up of immunoglobulin light chains.
This condition is distinct from other forms of amyloidosis (e.g., AA or ATTR) because:
- It arises from plasma cell dyscrasias.
- It has systemic effect, potentially involving several organs simultaneously.
- It possesses clinical characteristics in common with multiple myeloma but is different.
The Root Cause: Misfolded Light Chains
Underlying cause of AL amyloidosis is a plasma cell disorder, i.e., white blood cells that are in charge of antibody secretion. In AL amyloidosis patients:
- Plasma cells are clonal (abnormal).
- They secrete abnormal levels of monoclonal light chains (kappa or lambda).
- The light chains misfold and are unable to become soluble.
- Misfolded light chains are deposited as amyloid fibrils, which accumulate in organs and tissues.
These fibrils are toxic and they impair cells and tissues gradually.
How Plasma Cells Become Abnormal
The exact cause of plasma cell abnormality is not always clear, but several mechanisms participate:
- Genetic mutations in the bone marrow
- Chronic immune stimulation
- Random errors during B-cell maturation
- Abnormal immune response resulting in monoclonal gammopathy
The produced light chains are chemically unstable, which means they have a tendency to aggregate and form fibrils.
Monoclonal Gammopathy: An Important Contributor
What is Monoclonal Gammopathy?
Monoclonal gammopathy is a condition where an abnormal clone of plasma cells produces a monoclonal protein (M protein). The majority of individuals with this condition do not develop symptoms, but in others, it becomes a more severe disorder.
Types Associated with AL Amyloidosis:
- MGUS (Monoclonal Gammopathy of Undetermined Significance): A precursor state seen in most patients before they develop AL amyloidosis.
- Smoldering Myeloma: One step further toward multiple myeloma, but with no symptoms or organ injury.
- Multiple Myeloma: In a few instances, AL amyloidosis presents in combination with multiple myeloma.
NOTE: Not everybody with MGUS or multiple myeloma will develop AL amyloidosis, but these are known risk factors.
Risk Factors for AL Amyloidosis
Although the underlying cause is uncertain in most individuals, some risk factors predispose to developing AL amyloidosis:
1. Age
- Patients are usually diagnosed between the ages of 50 to 80 years.
- It is rare below the age of 40.
2. Sex
- AL amyloidosis is higher in males compared to females.
3. Monoclonal Plasma Cell Disorders
- MGUS or multiple myeloma are found in a significant percentage of individuals with AL amyloidosis.
4. Genetic Susceptibility
- Although not inherited, genetic predispositions in immune system control could raise risk.
5. Chronic Inflammatory Conditions
- Ongoing inflammation could abnormally stimulate plasma cells, although this is more associated with AA amyloidosis.
6. Environmental or Occupational Exposure
- Contact with toxins or chemicals impacting the function of bone marrow (like pesticides, solvents) could be loosely linked.
The Pathophysiology of AL Amyloidosis
Recognition of how AL amyloidosis occurs at a cellular level provides an understanding of its etiology.
Step-by-Step Development:
- Clonal Expansion: A few plasma cells turn clonal, i.e., they multiply uncontrollably and secrete one type of light chain.
- Light Chain Misfolding:These light chains do not have proper structure and are susceptible to misfolding, particularly under stress.
- Fibril Formation: Misfolded light chains produce beta-pleated sheet structures that are adhesive and cluster to form amyloid fibrils.
- Organ Infiltration: Fibrils accumulate extracellularly in organs and cause dysfunction and damage.
- Organ Failure: Chronic deposition results in fibrosis, inflammation, and ultimately organ failure, especially of the heart, kidneys, and liver.
Organ Systems Most Impacted
Its mainly involves:
- Kidneys: Resulting in nephrotic syndrome, proteinuria, and renal failure.
- Heart: Resulting in restrictive cardiomyopathy, heart failure, and arrhythmias.
- Liver: Causing hepatomegaly and liver dysfunction.
- Nervous system: Peripheral neuropathy, carpal tunnel syndrome.
- Gastrointestinal tract: Diarrhea, constipation, bleeding, and malabsorption.
The distribution of organ involvement is different between patients, so AL amyloidosis is referred to as the “great imitator.”
Diagnostic Clues to Uncover the Cause
Symptoms are nonspecific and resemble other conditions, so diagnosis is delayed. Diagnosis of the underlying plasma cell disorder, however, holds the key to knowing the cause.
Key Diagnostic Tests:
- Serum protein electrophoresis (SPEP)
- Urine protein electrophoresis (UPEP)
- Serum free light chain assay
- Immunofixation electrophoresis
- Bone marrow biopsy
- Tissue biopsy with Congo red staining
These procedures establish the monoclonal light chains are present, their type (kappa/lambda), and the degree of amyloid deposition.
Genetic Mutations: Are They a Cause?
Although its is not a genetic illness, bone marrow cell mutations that cause uncontrolled plasma cell growth are suspected to be involved.
Investigation is in progress into:
- Somatic mutations in plasma cells
- Epigenetic modifications associated with protein misfolding
- Heritable immune dysregulation, enhanced susceptibility
Knowledge of the genetic profile of AL amyloidosis might reveal individualized therapy in the future.
Global Epidemiology and Incidence
- Incidence per year: Around 9 cases per million worldwide.
- Prevalence: Estimated 30,000–45,000 patients have AL amyloidosis worldwide.
- Frequently underdiagnosed due to a delayed diagnosis or misclassification.
Countries with better diagnostic facilities (North America, Europe) have higher detection rates. Early diagnosis is difficult in low-resource environments.
Can AL Amyloidosis be prevented?
There is no definite method of preventing amyloidosis because its etiology is unknown. Yet, the following can be done to:
- Monitor high-risk patients (e.g., with MGUS)
- Treat comorbid conditions
- Educate primary care physicians about early warning signs
- Raise awareness to avoid delays in diagnosis
Raising Awareness: The Role of Education
Its awareness is low even among doctors. Misdiagnosis is frequent and expensive.
Here at amyloidosissupport, we are convinced that education saves lives. Here’s how:
- Public campaigns about orphan diseases
- Education of physicians through webinars and CME courses
- Outreach to the community to discuss risk factors and symptoms
- Patient testimonials to enhance identification of early warning signs
FAQs: Understanding the Causes
Is AL amyloidosis hereditary?
No. AL amyloidosis is not inherited, although some other forms (such as hereditary ATTR) are genetic.
Is AL amyloidosis the same as multiple myeloma?
Not exactly. Both are related to plasma cell disorders, but AL amyloidosis is caused by light chain deposition, whereas myeloma usually causes bone destruction and hypercalcemia.
Can MGUS transform into AL amyloidosis?
Yes. In some, MGUS can lead to AL amyloidosis or multiple myeloma. Monitoring is necessary regularly.
What causes light chain misfolding?
Specific causes are not known but could involve immune dysfunction, genetic mutations, or chronic antigen stimulation.
Final Thoughts: Knowing the Cause Is the Beginning of Healing
Its is a rare but curable disorder. Knowledge of its cause precursivum—abnormal light chain synthesis due to plasma cell dyscrasia—is key to early diagnosis and treatment.
By advancing research, increasing awareness, and advocating for patients on forums such as amyloidosissupport, we inch closer to improved outcomes, sooner diagnoses, and eventually, a cure.

