Case Report: Decline in Renal Function During Hospital Stay in a 61-Year-Old Patient with Amyloidosis
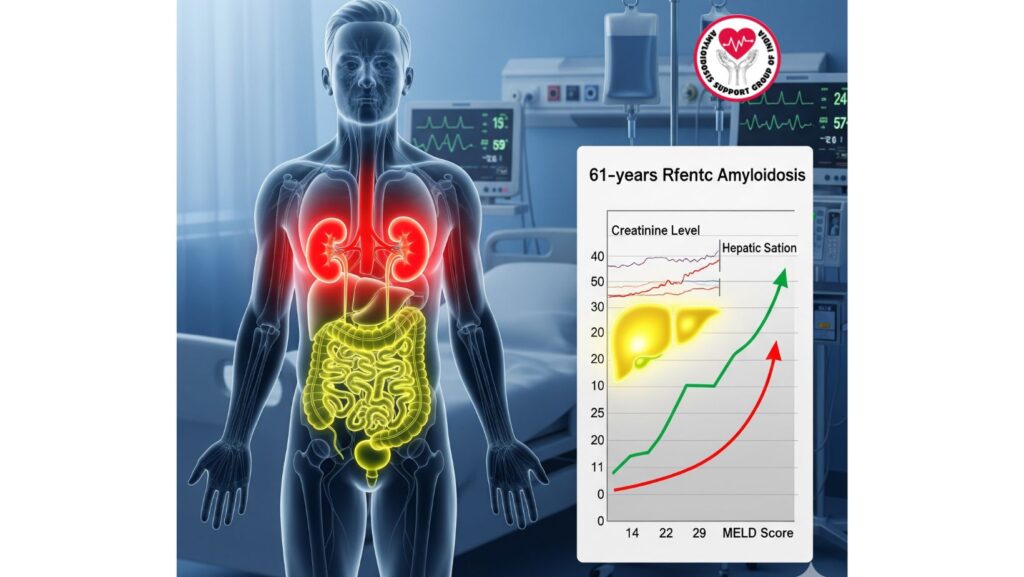
Table of Contents
Introduction
Amyloidosis is an uncommon systemic disease resulting from the deposition of abnormal proteins in multiple organs and causing progressive organ dysfunction. The kidneys are one of the most affected organs, wherein amyloid deposition results in proteinuria, nephrotic syndrome, and end-stage renal failure.
In this case report, we present a 61-year-old male patient with biopsy-proven AL amyloidosis who presented initially with hepatic dysfunction and ascites, but during his hospitalization, developed worsening renal function. This course illustrates the multi-organ nature of amyloidosis, the interaction between hepatic and renal illness, and the difficulty of managing such a patient.
Case Presentation
Initial Admission
The patient, an African-American male aged 61, was admitted with:
- Subacute abdominal distension and bilateral lower extremity edema (2 months duration).
- Tense ascites and jugular venous distension on physical exam.
- Laboratory findings such as hypoalbuminemia (2.1 g/dL), elevated alkaline phosphatase (718 IU/L), AST (158 IU/L), and ALT (119 IU/L).
- Normal bilirubin (0.5 mg/dL), normal INR (1.07), and normal creatinine (0.9 mg/dL) at baseline.
- Urine protein analysis disclosed nephrotic-range proteinuria.
Diagnostic Workup
- Viral and autoimmune panels: Negative.
- Imaging (CT abdomen): Ascites, potential nodular liver, no hepatosplenomegaly.
- Transthoracic echocardiogram: Left ventricular hypertrophy, concerning for infiltrative disease.
- Sigmoid colon biopsy: Congo red staining demonstrated amyloid deposits.
- Mass spectrometry: Peptide profile consistent with AL amyloidosis.
Hospital Course and Readmission
On Readmission
One month following discharge, the patient was readmitted with worsening ascites and new-onset jaundice.
Lab values revealed:
- Total bilirubin: 21.6 mg/dL
- Alkaline phosphatase (AP): 1317 IU/L
- AST: 260 IU/L
- ALT: 104 IU/L
A transjugular liver biopsy yielded amyloidosis without malignancy, fibrosis, or inflammation.
MELD Score
- Increased from 14 at baseline to 29 upon readmission.
- Suggested severe liver dysfunction with a poor prognosis.
Worsening Renal Function
Throughout the hospital stay, the renal function of the patient seriously worsened.
Clinical Indicators
- Increased serum creatinine levels above baseline (0.9 mg/dL → increasingly higher).
- Deterioration in fluid overload not completely accounted for by hepatic failure alone.
- Nephrotic-range proteinuria continued to indicate continued glomerular damage.
Pathophysiology
Amyloid accumulation in the kidneys classically happens in the glomeruli, blood vessels, and interstitium. This results in:
- Glomerular damage → heavy proteinuria, hypoalbuminemia, edema.
- Progressive renal insufficiency → increasing creatinine and decreased GFR.
- Interaction with liver disease → hepatorenal physiology complicating management.
Contributing Factors in This Case
- Multi-organ amyloidosis (hepatic + renal + possible cardiac involvement).
- Volume overload secondary to hypoalbuminemia and ascites.
- Hemodynamic alterations due to portal hypertension.
- Medication-induced nephrotoxicity and decreased renal perfusion during hospitalization.
Discussion
Kidney Involvement in Amyloidosis
- Nephrotic Syndrome: Heavy proteinuria (>3.5 g/day), hypoalbuminemia, and edema.
- Renal Insufficiency: Decreased filtration capacity due to amyloid deposition.
- Development of ESRD: Most patients will need dialysis if left untreated.
Prognostic Impact
- Renal impairment in amyloidosis significantly deteriorates survival.
- In addition to cardiac involvement, it is a key determinant of prognosis.
- Deterioration in renal function during hospital stay frequently indicates acceleration of disease.
MELD Score and Renal Dysfunction
- The MELD score measures liver disease predominantly but does not completely account for renal involvement unless MELD-Na is used.
- Here, the dramatic increase in MELD score (14 → 29) in conjunction with renal deterioration indicated systemic decompensation.
Management of Worsening Renal Function
Supportive Care
- Restriction of fluids and sodium to prevent ascites and edema.
- Diuretics (spironolactone, furosemide) with close monitoring of electrolytes.
- Infusion of albumin in selected individuals.
Specific to Amyloidosis
- Chemotherapy (bortezomib-based therapy) to decrease amyloidogenic light chains.
- Autologous stem cell transplantation in appropriate patients.
- Novel therapies against amyloid fibrils are in clinical trials.
Advanced Options
- Dialysis may be needed in progressive renal failure.
- Liver-kidney transplantation in selected cases of systemic amyloidosis, although the outcome is multifaceted.
Lessons from This Case
- Amyloidosis is a multi-organ disease – hepatic, renal, and cardiac manifestations usually occur together.
- Development of renal deterioration during hospitalization signifies unfavorable prognosis and narrow therapeutic window.
- Progression of MELD score alone does not reflect kidney dysfunction, but clinical monitoring is still crucial.
- Early treatment and diagnosis initiation (prior to the onset of multiorgan failure) is critical for survival.
- Multidisciplinary management (hepatology, nephrology, hematology, cardiology) enhances patient outcomes.
Conclusion
This case presents the aggressive course of AL amyloidosis with multi-organ damage. A 61-year-old male patient originally presented with liver dysfunction but went on to develop deteriorating renal function in-hospital, an indicator of disease progression.
Renal impairment in amyloidosis not only makes treatment more difficult but also has a major effect on prognosis. The dramatic increase in the MELD score (14 → 29) and worsening of renal function highlight the importance of early diagnosis, prompt treatment, and multidisciplinary care in the management of systemic amyloidosis.

